|
Hello you guys. It seems like a lifetime has passed since my previous post about traveling with children. In truth, it has been a lifetime. That was pre-2019 novel Coronavirus (COVID-19) and my oh my, things are really different. I don’t know where this post is finding you? Maybe you’re at your wits end as you juggle full-time parenting, full-time home-schooling, and full-time working from home? Maybe you or your spouse just lost your job(s) and you’re trying to figure out how you’re going to provide for your family? Maybe you or someone you love is sick with COVID-19 and you’re terrified of what’s going to happen? Maybe you’re feeling incredibly isolated and depressed? Maybe you’re one of those people who is enjoying this forced slow-down and you are savoring this extra time with your family? Or, maybe, you’re a little bit of all of the above. Whatever the case, and wherever this post finds you, I just want you to know I’m with you. Case in point: I started writing this post 2 months ago and it’s taken me this long to finish it! For all of you folks working from home with your kids at home, I give you major props because I can’t seem to get anything done right now. Times right now are hard, they are a bit scary, and we have no idea how long it will all last, which in my opinion, is the hardest part about all of this. Our job as parents is to protect and nurture our children and in these uncertain times many of us may feel like it’s hard to do this task well. My purpose for writing this post is to offer all you mommies and daddies out there some quick information and resources on COVID-19 that you can easily turn to from someone you trust if and when you need them.
So what is COVID-19 and why all the fuss? COVID-19 was discovered in late 2019 and in just 6 months it has spread like wildfire throughout the world. The biggest reason that health officials are so concerned about this virus is because it’s new and, therefore, very hard to predict what it will do. It is affecting some cities and communities more than others and has overwhelmed some health care systems. The symptoms of COVID-19 can range from mild to severe, with some people never showing symptoms at all. While most people who become infected will just have mild symptoms, some will be sick enough that they require hospital care, and many people have died. Symptoms typically begin about 2 to 14 days after exposure and include: cough, shortness of breath, fever, chills, repeated shaking with chills, muscle pain, headache, sore throat, and a new loss of taste or smell, with cough and shortness of breath being the most common. Thankfully, early data suggests that children are not at a higher risk of getting this virus and often show mild symptoms, if at all. They do seem to be affected a bit differently than adults as well, often not having a fever, cough or shortness of breath and most children do not need to be hospitalized. That being said, if your child suffers from an underlying medical condition like diabetes, lung disease or is immunocompromised, he or she is more at risk for complications from this virus. If your child is having flu-like symptoms and you think they might have COVID-19, especially if there has been recent travel to a high risk area and/or they’ve been around someone who has tested positive, it is recommended that they get tested. This is as long as your state has sufficient testing capabilities. Here in Utah, our testing capabilities have dramatically increased since the start of the pandemic and there are many options for testing including drive-up locations (see here). So, again, if your child is exhibiting symptoms, go get them tested. If you happen to live in a state where there isn’t sufficient testing and your child’s symptoms are mild, it’s recommended you stay home, isolate, treat symptomatically and monitor. Following COVID-19 testing, and especially if results are positive, it is important to isolate your child from the rest of the family as much as possible. They should stay in a room separate from the rest of the household, use their own bathroom (if toilet trained and if possible) and avoid sharing personal household items. I have a rule that when a stomach virus or pink eye is in the house, hand towels go out and paper towels move in. Now I’m adding COVID-19 to that list. In this new season, avoid hand towels (unless you can be sure each member will use their own) and use single use paper towels. Another option is to use hand towels once, throwing them into the laundry after every use. Isolating the sick family member obviously becomes complicated when you have a younger child, like an infant or toddler, who can’t be by themselves. If this is the case, one parent should isolate with the child and if the child is older than 2, he or she should wear a mask (as long as not having breathing difficulties) and the parent should also wear a mask at all times. Be sure to clean your hands often with soap and water or alcohol-based hand sanitizer. Also, clean all “high-touch” surfaces daily, this includes doorknobs, counter-tops, cabinet handles, remotes, tablets, computer keyboards, etc. Continually monitor your child’s symptoms and if symptoms worsen, call your child’s health care provider immediately. How long does your child need to isolate? Well, that depends. There are actually a bunch of different home isolation recommendations from the Centers for Disease Control and Prevention (CDC) depending on the situation, see here for the complete list. For the sake of this post, for the child that’s COVID-19 positive and symptomatic, then he or she can discontinue isolation when it’s been at least 3 days (72 hours) since resolution of fever without the use of fever-reducing medications and respiratory symptoms (e.g., cough, shortness of breath) have improved AND it’s been at least 10 days since symptoms first appeared. Again, depending on your circumstances the recommendations may be different, so please for the most current recommendations visit the CDC website or your local health department’s website. One of the questions I keep getting in clinic is the best way to prevent getting COVID-19. While we are learning more about this virus day by day and still have much to learn, I cannot stress enough the importance of hand washing, not touching your face AND practicing physical or “social distancing." You guys, I get it, we’ve been doing this thing for awhile now, it’s summer, we miss our friends and family, but we cannot go back to “normal” life yet. To help prevent the spread of this virus and protect the most vulnerable in our population, we HAVE to continue to practice social distancing. This means staying home as much as possible and avoiding group functions. This means saying no to that BBQ with a large group of friends and family, even if you’re the only family that does it. This means telling your school-aged son he can’t go to his friend’s bounce house birthday party. This means telling your teenage daughter she can't go shopping at the mall with her girlfriends. This means that if you must run an essential errand, you wear a face mask or cloth face covering. This means doing the hard things now, so we can get back to the things we enjoy safely later. There has been some controversy in the use of face coverings, which absolutely confounds me, but I really can’t recommend wearing them enough. You guys, this is a matter of community health and it shows respect to those around us. Let me put it another way: you wear a mask to protect me and I wear a mask to protect you and by doing so we are protecting our greater community which in turn protects us. Why? Since we don’t know who’s infected with COVID-19, especially if some people are asymptomatic or haven’t started exhibiting symptoms, and we know that airborne transmission is the most common route of transmission, we can decrease the spread by having everyone wear a face covering while out in public. Face masks or cloth face coverings are recommended for children for ages 2 and above, but they don’t need to be worn when at home (as long as no one in the family is sick) or outdoors as long as your child can maintain more than 6 feet between others and can avoid touching surfaces. I know this post just barely skims the surface of everything you may want to know, so please check out HealthyChildren.org’s page on COVID-19, which is powered by the American Academy of Pediatrics, and has great resources and information on all things COVID-19 and beyond to stay informed during this new and challenging season. Finally, please know we are here for you at ABC Pediatrics, and if you have any questions or concerns, please reach out and just give us a call. Take care of yourselves, stay safe and healthy, and wash your hands! Information presented adapted from: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/ https://www.healthychildren.org/English/health-issues/conditions/chest-lungs/Pages/2019-Novel-Coronavirus.aspx https://www.healthychildren.org/English/health-issues/conditions/chest-lungs/Pages/Cloth-Face-Coverings-for-Children-During-COVID-19.aspx https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html
3 Comments
Picture this: It’s January and you’re sitting on a beach with your toes in the sand and enjoying the sound of crashing waves as you stare out at the ocean and feel the warmth of the sun on your skin. Your baby of 6 months is napping on the towel next to you shaded by a sun umbrella and you smile as you watch your rambunctious 4-year-old playing happily with his dinosaur in the sand. Ahhhhh, vacation. What is not said in the aforementioned statement is what it took to get to paradise. There was saving, preparing, booking, planning, packing, driving, and flying. There were travel delays, tantrums, an in-flight "poo-plosion", and a forgotten toy. Nevertheless, you and your family persevered and here you all are (this is a true story, by the way, from yours truly). I often get asked about tips and tricks to travel with kids and whether or not it’s worth it. While the definition of vacation has changed with children, I would call it more of an adventure than a vacation. I’m here to tell you from experience, it’s always been WORTH it (see pictures below). I’ve broken up this post into three sections and I hope it helps inspire you and gives you the confidence to go explore our great big beautiful world.
PRE-TRIP: Once you’ve figured out where you’re going, it’s time to get excited and start doing your research as to what you’re going to need to do to prepare for your trip. A good place to start, especially if you’re traveling internationally, is to make sure your family is all up-to-date on all immunizations. Also, if you’re traveling internationally, you will want to make sure you don’t need any additional vaccinations in addition to the routine school immunizations. The Centers for Disease Control and Prevention (CDC) is a great resource for travel advice and needed vaccines (see here). You can also contact your local health department’s and make an appointment with a travel clinic. Finally, don’t forget to have your entire family get their flu shots if you’ll be traveling during flu and cold season. The more you can do to stay healthy and prevent illness, the better. It’s important to be organized with all of your trip documents. If you’re flying internationally, make sure each member of your entire family has a passport and that the passports aren’t due to expire for at least 6 months from your travel dates. If you have to apply for a passport, don’t delay, it can take awhile to receive them after your application is submitted. It’s also not a bad idea to make photocopies of your passports/IDs, health insurance card, travel itinerary and important phone numbers. Stash those away in a carry-on as well as your checked baggage. I’ve gotten in the habit of doing that, in addition to keeping those items in google document that I can pull up anywhere that I can connect to the internet. That way I have a paper copy (should the internet not be available) and another one that I can access digitally as well. PACKING: Packing for a trip is quite the task, but if there’s one thing I’ve learned over the years traveling it’s that less is more and to pack light. Yes, even with kids. You really don’t need as much as you think you do, especially if you’ll have laundry available. Of course, what you pack will depend on the time of the year you are traveling and your final destination. A trick I use is to always make a list prior to packing, that way I can check things off as I go and know I haven’t forgotten anything. About a week before the trip I start setting out piles of clothing and other necessities so I can easily visualize them and check them off finally as I pack them in their respective baggage. I also have gotten in the habit of packing an extra outfit or two for each person traveling (more if you’re traveling with an infant) and swimsuits in my carry-on. That way, should your checked luggage not arrive at your final destination or something unexpected happens while traveling, you’ll have something clean to change into. You guys, I can’t tell you how often this has saved me while traveling. If you are traveling with young children, make sure you bring along their car seats or arrange to have them at your destination. Many airlines will let you check car seats with no additional cost, but it’s not a bad idea to bring it on the plane for your child to use. Kids are safest when in a seat that is appropriate for their age, weight and height. If your child weighs more than 40 lbs, then he or she can use the aircraft safety belt. For those traveling with children less than 2 years of age and where purchasing an extra seat is not financially feasible, try to look into ways you could secure an extra seat for no additional cost. I always try to look into flights where it looks like there are a lot of empty seats and keep my fingers crossed that we can land an extra seat. Last, but probably most important, make sure you plan ahead if your child is taking daily medications like those for asthma or attention deficit hyperactivity disorder (ADHD). Make sure you have enough medication for the entire trip and always have it on your person, in other words, put it in your carry-on luggage, not in your checked baggage! You should bring Acetaminophen (Tylenol) or Ibuprofen (Motrin) with you as well just in case your child becomes ill enroute and make sure you know the appropriate dose for your child’s current weight. TRAVEL/FLIGHT: The big day is finally here and you are headed on your adventure. I know for most families, myself included, it’s the actual travel day that brings the most anxiety. This may be especially true if you’re traveling with an infant or toddler. You have visions of being “that family” on the flight whose child won’t stop screaming or throws a fit (Yes, I’ve been “that family” and I’ve lived to tell the tale). While I can’t promise you this won’t happen, what I can do is offer some suggestions to help avoid it or get through it. Make sure you bring plenty of distractions and snacks. One of my tricks is going to the Target dollar section or The Dollar Store and picking up a handful of random toys. I have found calculators to be a big hit as well as stickers and notepads. You would not believe how long you can entertain a preschooler as they try to finger tiny stickers onto a notepad. Make sure you don’t show these fun new toys to your kids until the flight and then you can pull out a new toy every 30 minutes or so (depending on the length of your flight) and hopefully it’ll provide some distraction. A colleague of mine also recommends wrapping up small toys that either your child loves or hasn’t seen in awhile. They will be thrilled at just opening it up (and recognizing their favorite toys) and others are obsessed with playing with the bows or wrapping paper. For snacks, pack a variety and pack things you know your children love. This not only saves you money in not having to buy overpriced airport or in-flight food, but gives you control over what your children are eating. I also recommend packing a few “special treats,” maybe some little candies, as rewards for listening and good behavior. You guys, I’m not above bribery when you’re just trying to get through a flight or long car ride-it works! From a health standpoint, I always recommend wiping down your seating area once you get on the flight with a wipe that has antifungal, antibacterial and antiviral properties. I personally use Clorox® Disinfecting Wipes On the Go (see here). You also want to bring plenty of hand sanitizer for when soap and water is not available. As you know, your kids touch EVERYTHING and then they stick their fingers in their nose or in their mouth or rub their eyes. Any effort you make in trying to minimize what they come in contact with is a good idea in my book. Nobody wants to be sick on vacation. Finally, the Benadryl conundrum. I often get asked whether or not it is a good idea to give children Benadryl while traveling. Forgive me for being so blunt, but NO. It is NOT a good idea to give Benadryl to your child while traveling. Benadryl is an antihistamine and recommended for those who suffer from allergies. Anytime you give a medication orally it enters the bloodstream and has a myriad of effects within the entire body. Benadryl given orally has effects on the brain, skin and gastrointestinal system. One of the more common side effects of Benadryl is sedation, meaning it makes you sleepy. I can see why some parents would find this effect desirable if they’re heading on a long flight hoping it might help their little one sleep, but the response to this medication varies from child to child, not to mention it can be harmful. Some unwanted side effects can include stomach ache, nausea, vomiting, dry mouth and, more rarely, an actual allergic reaction to the drug, heart palpitations, skin rash or other neurological changes. While some children may get sleepy on it, others can go completely bonkers. I’m talking “who are you and what have you done with my sweet child?” kind of crazy. This is called a paradoxical reaction. While a paradoxical reaction isn’t exactly harmful to a child, it’s definitely not something you want while traveling, especially confined on an airplane. One of our main roles as parents (and my role as a pediatric provider) is to protect our children. Anytime you use a medication not for its intended effect, you are playing with fire. We should never drug our children for our own convenience. I’m sure there are some pediatric providers (and parents) that may disagree with me on this topic and recommend this option to parents traveling with children. If that’s the case, please, do not try this method out for the first time while traveling. Practice first at home and make sure the dose you are giving is correct for your child’s weight. Also, NEVER use this medication in children less than 1 year of age (unless it’s being used for an allergic reaction under the direction of your child’s health care provider) as the sedation effect can have a much greater sedation response in younger children. Traveling with kids can seem daunting, believe me, I know (see below for some proof of travel photos!). It can seem especially daunting if you’ve never done it before. But, honestly, at the end of the day, it’s not anymore daunting than parenthood itself. Parenting is hard, wherever you do it. You might as well parent in fun and exciting new places from time to time, right? I can’t think of a greater gift to give your children than to discover new places and spend time with them as a family. Now, go EXPLORE! Information presented adapted from: https://www.healthychildren.org/English/safety-prevention/on-the-go/Pages/Travel-Safety-Tips.aspx https://wwwnc.cdc.gov/travel https://seattlemamadoc.seattlechildrens.org/if-it-were-my-child-no-benadryl-for-the-plane/ You guys, I have a confession. Well, maybe not so much of a confession as much as it’s an admission. I don’t do vomiting. The sound of retching and subsequent vomiting makes me turn on my heels and run as quickly as I can in the other direction. I am fully aware how this is somewhat problematic in my line of work because I evaluate a lot vomiting children, but most don’t vomit while I’m seeing them. Thank goodness! We all have our strengths and weaknesses, and my friends, vomiting is NOT my strength, I’ll admit it. I’m even more acutely aware of this after taking care of my sick toddler over the past week that culminated in vomiting. He didn’t even vomit on me. He vomited on my husband. But just the idea of being puked on had me dry heaving and rendered me useless in helping to clean up the mess. Diarrhea, no problem. Removing sticky, caked on boogers to the face, I’m a pro. Vomiting, no thank you. Taking care of a sick child is tough. Believe me, I know. When you add vomiting and diarrhea to the mix it’s not only tough, but it can be scary as well. Please read on to find out how you can help your children when they get stomach bugs and when you should worry and have him or her seen by their primary care provider (PCP). Vomiting is the forceful removal of stomach contents. It can be associated with or without diarrhea, which is two or more very loose or watery stools. Just having one loose stool is not diarrhea and can be totally normal from time to time. Both vomiting and diarrhea can be caused by gastrointestinal (GI) infection, either by a virus, which is the most common cause, or by bacteria. You can also get symptoms of vomiting and diarrhea from food poisoning which is ingesting contaminated food or while traveling. Have you heard of Montezuma’s revenge? Whatever the cause, vomiting and diarrhea can range from mild to severe and the biggest concern at the end of the day really is dehydration, which is what happens to your body when it has lost too much fluid. Most children with GI infections begin with severe symptoms and then will taper as they improve. For example, it’s typical of children with viral gastroenteritis to begin vomiting everything and not be able to keep anything down in the first few hours of illness. This can last anywhere from 3 to 4 hours, sometimes longer. From there, vomiting symptoms will decrease and they might have 1 to 2 episodes per day. Most vomiting will stop after 24 hours, but some children, especially younger kids, can have mild vomiting for a few days. After the vomiting subsides, many children will develop diarrhea or will have diarrhea with vomiting. Diarrhea can last days to even sometimes weeks. So what do you do when your sweet little one starts vomiting? First, don’t panic. While it’s terrible seeing them in that state, it hopefully won’t last for long. If they’ve thrown up over themselves or over their bedding, clean them up and get them into clean clothes and make a pile of dirty laundry for when you have time to get to it. That washer will be working overtime for the next few days. I then recommend either having a big bucket or deep bowl by the bedside and placing towels all over their bed and on the floor surrounding the bed. This makes for super easy cleanup if they miss that bucket. Another option is making a little bed of towels on the bathroom floor, but when you’re sick, it’s often times nicer to be in your own bed. Second, don’t let them eat or drink. Yes, you heard me right. During the first few hours of GI illness, what goes in, automatically comes right back out. Do yourself (and them) a favor and let those bowels rest for a few hours before offering anything. If they complain they’re thirsty, you can let them take sips of water, but make sure just sips, or ice chips if your child is old enough and not at risk for choking. Third, once your child has not vomited for a few hours you can then offer more fluids, but again, don’t let them do too much, too fast. I like to recommend ice pops or popsicles. It’s a way to hydrate them and give a little sugar, but because it’s frozen they don’t consume too much fluid too quickly. Finally, after they’ve kept fluids down for a few hours, you can them offer them food, but do so sparingly. Start with saltine crackers or toast and then add more foods as tolerated. If diarrhea is your child’s main issue, or it appears after the vomiting subsides, the no drinking rule does not apply. You can let them drink and eat as they please, but try to avoid fatty, heavy, or irritating foods. It is sometimes helpful to stick to the B.R.A.T. diet (bananas, rice, applesauce, white toast) because these foods act as binders and can help plug them up. Probiotics can also be helpful with profuse diarrhea, but be careful, in a few people probiotics can make diarrhea worse. Last, but certainly not least, horchata, also known as rice milk, is a great alternative to cow’s milk when your child has bad diarrhea. You can make it yourself (recipe here) or buy it at your local grocery store. The reason why I recommend avoiding cow’s milk in the days following a GI illness or with diarrhea is it can sometimes make diarrhea worse because the body can have trouble processing the lactose, which is the sugar found in milk. Most children will be mildly dehydrated after a GI illness. Don’t fret as this is easily fixed by pushing fluids. At what point should you worry and when is it time to make an appointment with me? Well, first, if at any point your child has decreased urine and does not urinate for more than 8 hours or if urine is dark yellow, it may be an indication of dehydration. Second, if you notice that their tongue is dry as well as the inside of his or her mouth. Don’t worry so much about dry lips as it’s not as good of an indicator. Third, if your child’s eyes are dry and they don’t make tears as they cry. Fourth, if your baby has a sunken soft-spot. Fifth, if you press on your child’s thumbnail and make it pale and let go and then count the seconds for it to turn pink again and it takes longer than 2-3 seconds refill. Sixth, if your child is acting really sick, lethargic and is too weak to stand or, alternatively, if he or she is inconsolable and you can’t calm them down. These are all signs of dehydration or worsening illness and he or she should be been by their PCP immediately. Finally, I’d like to leave you with a few more pointers and things I’ve learned taking care of my own sick kids. When there is vomiting or diarrhea in the house it’s time for paper towels, bleach and lots of handwashing. You guys, I’m all about saving the planet, but to help protect others in the family from a similar date with the porcelain goddess, ditch the hand towels and do single use paper towels in the kitchen and bathrooms for a week. Clean all household surfaces with diluted bleach water as this is the most effective way to kill some of the most virulent stomach viruses. Finally, wash those hands!!!!! In a pinch, a dollop of your hand sanitizer is a good option, but the best way to prevent illness is to thoroughly, and frequently, wash your hands with soap and water. My hope is that your little gal or guy is feeling better in no time and the rest of your family can get through it all relatively unscathed. Vomiting and diarrhea are no fun, but with this knowledge you will get through it. And, please, know that I’m here for you for all those questions and everything in between. Information presented adapted from : https://www.healthychildren.org/English/tips-tools/symptom-checker/Pages/symptomviewer.aspx?symptom=Vomiting+With+Diarrhea https://www.cdc.gov/norovirus/about/index.html Fall is in the air folks. The heat of the summer is giving way to cool and crisp mornings and I could not be more excited. Fall to me means pulling out those cozy sweaters, sipping on warm drinks, enjoying pumpkin spice treats and being amazed by the changing landscape from vibrant greens to fiery yellows, oranges and reds. It also means Halloween is right around the corner and, if you are the parent of little ones, there are few holidays that bring more joy (and cuter photo opportunities) than Halloween. Right now you may be in the midst of deciding on costumes, so I'm hoping that this post crosses your path at just the right time. While Halloween is super fun, we also want to make sure you know how to keep your kiddos safe for trick-or-treating. When choosing your child's costume, make sure you choose a costume that is well-fitting and age-appropriate. You want to be sure that it's free of anything that could be hazardous like it being too long of a length that they could trip over; a sword, cane or stick that goes along with the costume that they could accidentally be hurt by; or a hat that's too big and blocks their eyesight. Speaking of eyesight, it would be a good idea to consider using non-toxic make-up instead of using face masks as those can often block your child's line of sight. Just be sure to test out the non-toxic makeup ahead of time to avoid any skin reactions on the big day. When buying a Halloween costume or accessories, make sure the label reads “flame retardant/resistant”. It may also be a good idea when picking out a costume, if possible, to choose bright colors or to add reflective tape to it or their treat-or-treat bag that will help make them more visible to motor vehicles and other people. Finally, it can be hot or cold on the night of trick-or-treating and it’s always a surprise what mother nature decides to do, so make sure your child is appropriately dressed for whatever she decides. If pumpkin carving is part of your family's Halloween tradition, make sure that young children never do the carving. Have them draw a face or design and then you can do the actual cutting. Most kids don’t care to do the carving anyway, the real fun is getting to grab the squishy and gooey pumpkin contents. Also, don’t throw away those seeds; after separated and rinsed, you can bake those pumpkin seeds and they are delicious, healthy snack. If possible, avoid using real candles to light up your pumpkin as this presents a fire hazard. If you need to use real candles, votives are the safest. In addition, be sure to place your beautiful masterpiece on a sturdy table, especially if using real candles. Now for the main event: the night of Halloween and trick-or-treating. Try to offer your kiddos a good meal prior to going out; this will ensure they don’t fill up too much on those goodies. A parent or responsible adult should always accompany young children trick-or-treating. If your child is old enough to trick-or-treat alone, which depending on the responsibility and maturity level of your child is usually between the ages of 10 and 12, be sure that they go in a group, as well as assign a buddy within the group. Review the route that is acceptable to you and the specific time they should be home. Also review how to call 911 in the event of an emergency or if they become lost. Be sure that all trick-or-treaters and their chaperones have a flashlight with fresh batteries. Only visit homes that have a porch light on and never, ever go into a home or car for candy. Always walk on sidewalks and well-lit streets and, if no sidewalk is available, walk along the farthest edge of the roadway. Do not cut through yards or alleys and always cross the street using crosswalks. Also, do not assume that you have the right away, many times drivers cannot see you; stop, and if you see an approaching vehicle, wait until the roadway is clear before crossing the street. At the end of the evening, wait until you are home to go through your child’s Halloween loot and throw away any spoiled, unwrapped or suspicious items. Once sorted, you can give the stash back to them--but, if the idea of them on a non-stop sugar high for the next week makes your skin crawl, you can try one of the following ideas:
Information presented adapted from: https://www.healthychildren.org/English/safety-prevention/all-around/Pages/Halloween-Safety-Tips.aspx For those of you that read this blog, I’m sure you’ve noticed it has been radio silence on my end for about one year. Let me first apologize for my hiatus, but my friends, LIFE has happened. The full-human experience: the crazy, the heart-breaking, the miraculous and the beautiful. It is only now that I feel like I’m coming up for air. I will give you fair warning, this post is getting personal. Why? Well, I teetered for a while on this one, but I felt that I owed it to my patients and their families to be real and honest. Not that I wasn’t doing all these things before, but I could have just picked right up where I left off without mentioning what has gone on in my personal life this past year and I decided I didn’t want to do that.
When I started this blog four years ago, I wanted a resource for my patients and their parents that would provide accurate and straightforward information on common pediatric problems and give general parenting advice. I know from personal experience that when you’ve lived something that others have lived, you become more relatable and what you say is taken more to heart because you've been there. As a new practitioner, and before having children of my own, I gave parenting advice as best I could. My education and training gave me a good base, but no amount of education or training could prepare me for the moment I welcomed my first son into the world four years ago. As a new parent, I entered into the same ranks as my patients’ parents. I immediately had more credibility as I knew what it meant to love and care for a child: the fears, the joys, the highs and the lows. I want you to know that this blog is not only written from the perspective of a Pediatric Nurse Practitioner, but also from the perspective of a mother, a sister, a daughter, an aunt and a friend. What you read here will not only be accurate and evidence-based, but it will also come from the heart. Approximately 1 year ago, my mother passed away peacefully after a long and valiant battle against breast cancer. Less than 3 weeks later, I gave birth to my second child, a sweet baby boy. In less than 1 month, I witnessed life leave this world and witnessed life enter it. I went from overwhelming grief to overwhelming joy and my life was turned upside down. Looking back, it is all a blur. Nevertheless, the reason I mention any of this is that through it all, I had a very inquisitive and tender 3-year-old son who was also trying to make sense of everything that was going on. He had questions like “Where is yaya (my mother)? What is heaven? When I'm sick does that mean I'm going to die? Mommy, are you going to die too?” These are only a select few of the myriad questions he had, many of which I had trouble answering. You guys, I'm a Pediatric Nurse Practitioner, I'm supposed to know what to say in these situations, and I struggled. I felt I was often coming up short. I hope that you never have to have these tough conversations with your children. These are the kind of conversations that break your heart and bring you to your knees, but if you do, I hope this post makes them easier for you. And, my deepest sympathies to you as you grieve for that special person in your life who is no longer here. I'm so sorry for your loss. So what do you say to your child after someone close to you has died? Where do you even begin? This all depends on your child’s age. Your toddler isn’t going to comprehend death in the same way your teenager will, so, the method you choose to explain death will depend upon your child's age. If you have an infant or toddler in the house, know that they will not understand that someone has died as they can’t comprehend death, but they will pick up on what you and other loved ones are experiencing. Let yourself grieve and know that it is okay to let them see you when you do. This is actually true for all ages. Grief is a funny thing sometimes, it sneaks up on you when you least expect it, so if and when you have a moment in front of them know that it’s fine. Hold them close and tell them you are okay, you are just missing whoever has died. Try your best to keep to a typical daily routine as this provides security for your child. If you can, avoid being separated from your children during this time and give more physical attention. Hug them, kiss them, and hold them. This not only comforts your child or children, but I promise it will comfort you as well. For those with a preschooler in the home, know that they view death as a temporary thing. It is important to give these concrete thinkers clear and simple explanations to what has happened. Avoid euphemisms like “He went to sleep” or “She is gone”. To your three-year-old “He went to sleep” becomes “when is he waking up?” Or, “She is gone” becomes “Where did she go?” Instead, tell them simply “Your grandma has died and that means we no longer can see her anymore.” These straightforward answers can be softened by reminding your child that they will always have memories of the loved one who has died. Finally, don’t be surprised if they will randomly bring up the person who has died, sometimes weeks or months after they’ve died. You may also see this in their play, so pay attention. If your child, all of a sudden, has a new-found obsession with his plastic dinosaurs dying as my son did—this could be his way of expressing your loved ones death. Continue to provide support and encouragement. School-age children may be able to understand that death is final, but they may not be able to comprehend that death is universal. It is best to be simple and honest with your explanations about what has happened and then be sure to ask them if they understand or have questions. It is also important to clear up any misconceptions. Your child may have trouble expressing his or her emotions. Try to listen more than offering words, give your support and repeated opportunities for them to express how they are feeling. Your child may also worry they will be left all alone. My son repeatedly asked me if I was going to die after my mother died, this was especially true when I was leaving for the hospital to have his baby brother. The fact that I was going to the hospital made him worry I wasn’t coming back because this was true of his grandma. Again, clarifying to your child that not everyone who experiences sickness progresses to death will help them, as will explaining that not everyone who goes to the hospital dies. Reassure your child of your health and that there are many people in their life that care for them. This should help ease their anxiety. Be patient, it’s a process. Your teenager is going to understand death in the same way an adult does but they may resist expressing any emotion about it. He or she is now able to think more abstractly and may start having some big questions into the meaning of life or futility of it. Do your best in answering these questions and supporting them. They may also rebel a little and participate in risky behavior, which is typical of teenagers. Try to be a model of healthy ways of grieving, be present, and keep them accountable. Whether you have babies, teens or are somewhere in between, experiencing the death of a loved one and discussing it with your children is no easy thing to navigate. Let your love be your guide. Be sure to be patient and be honest with your children. You will get through it. Life does carry on. Believe it or not, your heart will ache a little less with each passing day and your children will be lucky to have you there helping them through it as you are lucky to have them helping you. Hang in there and keep on, keeping on. Information presented adapted from: https://www.healthychildren.org/English/healthy-living/emotional-wellness/Building-Resilience/Pages/How-Children-Understand-Death-What-You-Should-Say.aspx If you are currently raising a teenager, you might be noticing that he or she is going through a slew of changes at the moment. They may be going through a growth-spurt and their bodies are beginning to change, they may have an insatiable appetite and you feel like they are eating you out of house and home, they may be more moody or sensitive and some days you may wonder if even know them at all. All of these changes are a part of puberty and while some changes can be exciting for your teen, there are plenty of changes that are annoying, like acne. As someone who dealt with acne as a teen herself, I completely sympathize with my patients who are frustrated by problem skin. When I first started at ABC Pediatrics 5 years ago, I realized that many of my teenage patients had questions about acne and how they could treat it. Because of this, I created a hand-out to summarize the acne information I go over during the adolescent visit (see here) and this post is a summary of that. Please read on to see how you can help your teen if they are suffering from acne.
So what is acne anyway? Basically, it is when the pores in the skin become clogged and infected. The skin has tiny pores which contain hair follicles and glands that produce oil to lubricate the skin and hair. During puberty, oil glands sometimes will make too much oil. This, along with dead skin cells, can cause a plug to form that clogs pores and causes acne. Furthermore, this plug attracts bacteria that can cause inflammation. There are three forms of acne: blackheads, whiteheads and pimples or cysts. Blackheads (open comedones) form when a pore is clogged, but stay open. Whiteheads (closed comedones) form when a pore is clogged and closes up. Finally, pimples or cysts are inflammatory lesions meaning that once a pore is clogged and closes up it can become infected. Acne is treated by performing good skin hygiene and using medication(s) that help to unclog pores, reduce the number of bacteria on the skin and decrease or stop excess oil production. There are over-the-counter medications that can be helpful for milder cases of acne, like benzoyl peroxide, but if those are tried, and there is no improvement or worsening, it may be time to seek medical advice and make your child an appointment with his or her primary care provider. It is important to have a good skin care routine as well. Make sure your teen is gently washing (not scrubbing) her face with a mild cleanser at least twice a day and then splashing her face with cool water and patting (not rubbing) dry. I find that many teens are excessively scrubbing their skin which can cause further irritation and makes things worse. If your teen is using an acne medication, apply it sparingly to affected areas as directed. It is important to stress to your teen that they need to give things time to improve. Unfortunately, there is no magic, overnight fix. To make matters worse, acne often gets worse before it gets better, especially when starting an acne medication. The time frame typically goes like this: things usually worsen around weeks 1 to 2 into treatment and then things gradually improve from there. Your teen should allow up to 8 weeks to see a difference in her skin. It is sometimes helpful to take a weekly photo and you can both monitor progress (this helps your practitioners out as well!). Make sure that any lotions and/or make-up your teen puts on her face are “non-comedogenic” (meaning it won’t clog pores). Finally, if your teen participates in sports or is very physically active, make sure that she washes her face after activity as well as in the morning and evening before bed. Having acne is hard, but it is not hopeless! There are plenty of treatment options available to help your teen move towards clearer skin. Still have questions or maybe one that is more specific to your teen’s situation? Please do not hesitate to contact us at ABC Pediatrics if we can be of further assistance. We are happy to help! Information presented was adapted from: https://www.aad.org/practicecenter/quality/clinical-guidelines/acne https://www.healthychildren.org/English/ages-stages/teen/Pages/Teens-and-Acne.aspx Media screens. They are EVERYWHERE. You probably don't go through a single day without looking at some form of digital media as they have become ubiquitous in our culture and are often necessary to get through a typical day. This also means they are likely ever present in the lives of your children, or, if they aren't yet, they will be. Because of this, it is very important, as a parent, to know how digital media impacts your children and their development and what experts are recommending for proper use of screen time.
Let me first start by saying that while there are definitely negative aspects of digital media to the health and development of children, there are plenty of positives. The aim of this post is to help parents be more aware of how digital media affects their child (and themselves) and the best ways to incorporate it into their daily lives. The idea is for digital media to be complementary, not detrimental. Here are the recommendations:
So what happens when there aren’t restrictions placed on media use? There is concern that heavy use of media, especially during the preschool years, is associated with an increase in body mass index (BMI) and may increase that child’s risk for obesity later in life. There are also negative effects on sleep, especially when media is used prior to bedtime or when electronics are in the bedroom. There is also an association between fewer minutes of sleep per night when there is a television, computer or mobile device in the bedroom (that goes for adults too!). I don’t know how many times I’ve seen children in clinic who have difficulty in falling asleep at night and one of the first questions I ask is about screen use before bed and whether or not there are electronics in the bedroom. This is the first thing that needs to be changed and is often the solution to the problem in most cases. There also have been population-based studies that show an association between heavy television viewing in early childhood and social/emotional, cognitive, and language delays. Screens cannot take the place of what our children need from us for proper brain development — our presence. Hands-on, unstructured, and social play is essential to build language, cognitive and social-emotional skills. Things like task persistence, controlling of impulses, emotional self-regulation, and creative, flexible thinking are taught best by social and unstructured playing and through a responsive parent child interaction, not through a digital screen. In summary, digital media should not get in the way of activities essential for proper child development such as playing, sleeping, being physically active, down-time and time spent as a family. I also get a lot of questions in clinic from parents, not only about what an appropriate time limit should be for viewing digital media, but also regarding the content of what their children are watching or playing on their screens. As a parent myself, I’m aware that there is a dizzying sea of available programs, movies, games that are accessible all day long. Knowing what is appropriate for your child isn’t always easy to figure out. Well, Common Sense Media to the rescue (see here)! Common Sense Media is a non-profit organization that is committed to providing unbiased information so that parents can decide what media is right for their family. They do the work of figuring out what is developmentally appropriate so you don’t have to. So what happens if bad habits are already in place? And, what happens if you realize you, as the parent, may have a problem with media use yourself? The answer is, it’s never too late to change. And, the good news is, your children are learning by your example, so if you show responsible digital media use, they will too. The American Academy of Pediatrics (AAP) has a handy Family Media Use Plan that helps you and your children to think about media and create rules and goals that align with your family’s values. Fill it out and then print and place it where it’s visible to the entire family. It’s a great tool to make sure that in this digital age, we are being responsible media users and we don’t let technology get in the way of what matters most, the health and well-being of our families. Thanks for reading, until next time! Information presented adapted from: http://pediatrics.aappublications.org/content/early/2016/10/19/peds.2016-2591 http://pediatrics.aappublications.org/content/early/2016/10/19/peds.2016-2592 http://pediatrics.aappublications.org/content/140/Supplement_2/S57 https://www.aap.org/en-us/about-the-aap/aap-press-room/pages/american-academy-of-pediatrics-announces-new-recommendations-for-childrens-media-use.aspx Microorganisms are everywhere and are an essential part of our existence. Some carry the potential for harm, like germs that make us sick, but many others have the potential for good, such as probiotics. These particular microorganisms have gained a lot of attention in the past decade and have become quite the buzzword. There is a lot of interest and ongoing research on how our gastrointestinal (GI) flora affects our everyday health and whether or not taking probiotics can improve our health. Proponents of probiotics claim a myriad of health benefits as well as the prevention and treatment of diseases. So, what does that mean for your child and should you be giving him or her a daily probiotic supplement? Well, please allow me to help you decide what might be right for you and your family. Read on to find out more information about the use of probiotics and whether it is right for your child.
Now, in order to understand what probiotics are, it is helpful to understand your microbiome (i.e. the bacteria that inhabits our bodies) in general. Large numbers of microorganims live in and on the body. In fact, these bacteria outnumber human cells by 10 to 1. Bacteria are normally present in our intestines as well because they help us digest the food we eat, they kill microorganisms that cause disease, and they produce vitamins. At birth, infants have a sterile GI tract and that quickly changes with bacterial colonization. The gestational age of the infant, the way in which he or she was birthed (C-section vs. vaginal), and the infant’s diet all influence this process of bacterial colonization. After infancy, the GI flora doesn't change much. The intestinal mucosal defense system is an essential part of a complex immunoregulatory network that includes GI microflora. It is a widely held belief that the incidence of many diseases, both intestinal and non-intestinal, are related to impairment in the regulation or interference with the early development of the intestinal mucosal defense system. So then, what is a probiotic? A probiotic is any food or oral supplement that contains enough microorganisms to change the microbiome of the person ingesting them with the potential for improved health. The most studied strains to date are Lactobacillus rhamnosus GG (LGG), Bifidobacterium lactis, and Streptococcus thermophilus. You may recognize these names if you're a food label reader like me. Probiotic bacteria can be ingested as a medicine or as a supplement. They can also be added to or mixed with foods or naturally exist in functional foods, which is any food that contains a probiotic, like yogurt or kimchi. Many parents have asked whether or not probiotic supplements are okay if given daily or if they could be helpful for their infant's colic? As mentioned above, the use of probiotics in the prevention and treatment of clinical diseases is an emerging science, meaning there is still much to learn regarding the benefits and potential dangers that may exist. There have been well-conducted randomized controlled trials (RCTs) to support the use of probiotics for the treatment of acute infectious diarrhea. One study suggested that the administration of LGG significantly decreased the duration of acute rotavirus diarrhea. At this point, however, there is no evidence that routine use of a probiotic prevents acute infectious diarrhea. There have also been other studies that suggest probiotic use in the earliest phase of illness not only decreases the duration, but also the amount of diarrheal stools. Probiotics have also been useful in the prevention of antibiotic-associated diarrhea. To date, there haven't been any studies to investigate probiotic administration in the treatment of antibiotic-associated diarrhea. There also is a lack of evidence for the efficacy of probiotics for many diseases such as eczema, chronic inflammatory bowel disease, irritable bowel disease, infantile colic and cancer. That being said, just because there is a lack of evidence currently, does not mean that with further study, potential benefits won't be established. However, for right now, the area in which probiotics have shown the greatest benefit is with the treatment of acute diarrheal illness and the prevention of antibiotic-associated diarrhea. So what does this mean for your child and should you give him or her a daily probiotic supplement? As long as your infant or child is healthy, probiotic supplements seem to be safe. Furthermore, they seem to be beneficial in treatment of acute diarrheal illness and prevention of antibiotic-associated diarrhea. Patients that should NOT take a probiotic unless directed by their primary care provider are those who are immune-compromised; this includes ill preterm neonates and children who have intravenous catheters or other indwelling medical devices. I hope this post was informative and answered some questions you had about probiotics. Please contact us at ABC Pediatrics if you have any further questions. Information presented was adapted from: http://pediatrics.aappublications.org/content/126/6/1217 https://nccih.nih.gov/health/probiotics/introduction.htm October is National Bullying Prevention Month where communities across the nation try to bring awareness to this persistent and pervasive problem. By now, kids are fully back into the swing of school and that can mean they are back at a place where they can be bullied or are taking part in bullying. I, along with many fellow colleagues, try to make it a point during each well-child check to ask about bullying and ways to prevent it. Despite that, if your kids are generally healthy, your child’s primary care practitioner (PCP) only sees them once every one or two years and that is not often enough to be screening for bullying. This should be done regularly because things can change in an instant. It is important as parents that we know what bullying is, how to recognize it, tangible ways to tackle it, and, heaven forbid, what to do if your child is the one doing the bullying.
In order to identify if your child is being bullied, you have to first know what bullying is. Many people have varying definitions of bullying and situations that may seem like innocent teasing to some are actually bullying to others. Which one of the following scenarios could be classified as bullying?
If you answered that all of these scenarios could be considered bullying then you are correct. Some of the scenarios listed are even instances of assault, but that goes beyond the scope of this post. Bullying is when a person picks on another person, over and over again. Typically, children who are bullied are small and weak, they often are shy, and they often feel like they have no control over the situation. However, these are by no means the only criteria. Bullying differs from teasing in that the person doing the bullying has control of the child being bullied and this is often done by scaring them, making them feel like the victim, especially because this is often done in front of other children. There are three different kinds of bullying: physical, verbal and social. Physical bullying is using actual force by hitting, kicking, pushing, punching or choking. Threats, taunting and teasing comprise verbal bullying. Social bullying can be anything from, 1) not including someone in social activities on purpose, 2) posting something negative about someone on social media and 3) spreading rumors about someone around school. Bullying can happen anywhere, but more often than not, it takes place at school, often when adults are not around, and through electronic means via texting, email or social media. So how do you get your child to open up about possible bullying? Well, try open-ended questions. These are questions that make your child respond by saying more than yes or no, or, if you currently are raising a teenager, more than a grunt or an eye-roll! Try asking them how things are going at their school? Or, what do they think about the people at their school? Better yet, get to the point and ask them if they’ve witnessed any bullying or teasing at their school? This gives your child an opportunity to really open up about their school life in general, and, even if you don’t discover your child is being bullied, you may find out other information such as your child is struggling with a certain class or feels nervous about an exam that’s coming up. If you do find out that your child is being bullied, make sure you teach your child how to stay safe (see here) and how to handle a bully if it happens again. Now, just teaching your child what to do or say often isn’t enough. These things often require practice and role-playing. Furthermore, they are often things that don’t come naturally to the child being bullied, so practice until it becomes second nature. For example, teach your child how to be confident physically (i.e. look the bully in the eye, stand tall, be calm, stand their ground, and if needed, how to walk away). Teach them what to say and how to say it (i.e. “I don’t like what you’re doing” or “Please do NOT talk to me like that” or “Why would you say that?”). Many times, just the fact that the person being bullied stood up to the aggressor is enough to make the bullying stop. Again, bullies often prey on those who appear weak, so if your child show strength and evens the playing field, it can stop. It is also important that your child knows when to seek help and you should always alert school officials that bullying is going on. They can’t fix the problem if they aren’t aware anything is happening in the first place. So what to do if your child is the aggressor? First, don’t blame yourself, but make sure you take it VERY seriously. You don’t want to ignore this behavior and hope it goes away on its own. Things often get worse if not dealt with as soon as the behavior is discovered. You want to be sure to that your son or daughter knows that bullying is never OK and make sure that all aggressive behavior is limited and dealt with on a consistent basis. Make sure your child knows that he or she can get what they want by being respectful to others. They never to need to resort to coercing or threatening someone. Be a positive role model for them and discipline them by using effective, non-physical means and/or loss of privileges. Work with the school, teachers and other adults, to develop ways to prevent these instances happening in future. Finally, try to have your child put themselves in another person’s shoes. Showing them that bullying hurts is often enough to make them stop what they are doing. Also, make sure they know that they should stop bullying if they ever see it happening to another person. Burger King got this SO right with a recent bullying prevention ad-campaign. Honestly, you could start the conversation by just having them watch this. Please contact us at ABC Pediatrics if you have any questions or concerns regarding bullying or any other health concerns. We are happy to help! Information presented adapted from: https://www.healthychildren.org/English/safety-prevention/at-play/Pages/Bullying-Its-Not-Ok.aspx https://www.healthychildren.org/English/safety-prevention/at-play/pages/Avoiding-Bullying.aspx It's back to school time and if you are the parent of a child just starting middle school, that means it's time for his or her middle school set of vaccinations. I have had some parents ask about the human papillomavirus (HPV) vaccine which isn't required for entrance to middle school, but is highly recommended. In my professional opinion, I feel that it should be required and it is my hope that after reading this post you will see why I feel strongly about this cancer-preventing vaccine.
Human papillomavirus is a virus that is most commonly acquired through sexual contact. In fact, it’s the most common sexually transmitted infection (STI). HPV infection is so common that almost everyone will be infected at some point in their life. According to the Centers for Disease Control and Prevention (CDC), approximately 79 million Americans are currently infected with HPV and there are 14 million new cases each year. In many cases, fortunately, HPV will go away on its own and not cause any long-term health problems, but when it doesn’t, it can cause genital warts and cancer. The most common cancer caused by HPV infection is cervical cancer, but it can also cause cancers of the vagina and vulva in women, cancer of the penis in men, and cancers of the mouth, throat and anus in both men and women. The scary thing is most who are infected with HPV aren’t even aware they have it and it can take years for someone with it to develop cancer. Prior to the HPV vaccine, the only ways to prevent acquiring HPV and the health problems it can cause was to use protection such as latex condoms if sexually active, but even that can't offer full protection. Other means to prevent it are 1) to be in a mutually, monogomous relationship and, 2) to be screened for cervical cancer if female. Fortunately, now (well, actually for the past decade), we have another means of prevention and that's through the HPV vaccine. There are over 100 different strains of HPV and while the HPV vaccine doesn't protect against them all it can prevent infection from the more high-risk strains. The HPV vaccine can prevent cancers caused by HPV Types 16, 18, 31, 33, 45, 52, and 58. It also can prevent precancerous lesions caused by HPV Types 6, 11, 16, 18, 31, 33, 45, 52, and 58; as well as genital warts caused by HPV Types 6 and 11. Now it is important to mention that not all cancers of the vulva, vagina and anus are caused by HPV and the HPV vaccine only protects against the strains aforementioned. The HPV vaccine is approved by the food and drug administration (FDA) and is recommended by the CDC for females and males between the ages of 9 and 26 years of age, although it is routinely given at 11 or 12. One of the questions I have received in clinic is, “Well, my child is only 11, and he isn't sexually active nor is he going to be anytime soon. Why does he need this vaccine now”. The answer is simple. The idea of vaccines is to protect your child long before they will exposed to the disease, – so in the case of HPV, long before he is ever sexually active. For example, we don't wait until your child is exposed to measles to protect him from it. This is the same idea with the HPV vaccine. In addition to that, preteens have a more vigorous immune response to HPV vaccine as compared to older teens. Your child will only need two doses if vaccinated before the age of 15 versus the three doses if vaccinated at 15 or older. Another concern I have heard from parents is the idea that the HPV vaccine is too “new” to the vaccine schedule. In all honesty, it's really not. Yes, it hasn't been around as some of the other routine vaccines, such as the Measles, Mumps and Rubella vaccine (MMR) and the H. influenzae type B vaccine (Hib), but it still has had years of clinical trials and post-marketing safety surveillance data to show it's safe and effective. The HPV vaccine was first developed in Australia over 20 years ago and filed for U.S. patent in 1994. In 2006, the FDA approved the first preventive HPV vaccine and by 2008, over 80 countries across the world had approved it. Since then — about a decade now— it has been approved in over 100 countries with over 100 millions doses given world-wide. You can also look at it this way, if your child is entering middle school, the vaccine is older than your child; it's really not that new. Just like the other vaccines your child will be receiving at his middle school well-child check, the HPV vaccine is safe and effective. No serious side effects have been caused by the HPV vaccine, but as with any vaccine (or medication), there is always a risk for side effects, even serious ones, like allergic reactions, injury or death. The most common side effects associated with the HPV vaccine are just local site reactions like mild redness, swelling or pain at injection site. Some patients experience fever and others have complained of a headache, but overall, it is very well-tolerated and these symptoms should go away quickly. To date, the HPV vaccine has not been associated with any long-term or serious side effects. The benefits of this vaccine far outweigh the risks. Moreso, the HPV vaccine is effective. In Australia, where they have a National HPV Vaccination program and have had better rates of vaccination against HPV, there has been a significant decrease in HPV-related infections in young women. In fact, an October 2012 study in The Journal of Infectious Disease found that the prevalence of vaccine-preventable HPV types (6, 11, 16, and 18) in Papanicolaou test results of women aged 18-24 dropped significantly from 28.7% to 6.7% — only four years after the National HPV Vaccination started. In addition, the vaccine is long-lasting and there is no evidence of waning immunity for at least 10 years. Now, as far as how long immunity lasts after inoculation, that is still unknown. It is my hope this post has helped inform you regarding the HPV vaccine and allay some worries you may have had. I strongly believe in the importance of this cancer-preventing vaccine, why I'm talking about it here and why I recommend it to all my patients. What's more, we at ABC Pediatrics, believe that vaccinating your child may be the single most important health promoting intervention we perform as health-care providers and that you can do as parents and caregivers. As always, do not hesitate to contact us if you want any more information on the HPV vaccine or with any other questions or concerns. We are happy to help! Information presented adapted from: https://www.cdc.gov/std/hpv/stdfact-hpv.htm https://www.cdc.gov/vaccines/parents/diseases/teen/hpv.html https://www.healthychildren.org/English/safety-prevention/immunizations/Pages/HPV-Gardasil-9-What-You-Need-to-Know.aspx https://www.google.com/patents/US7476389 https://www.merckvaccines.com/Products/Gardasil9 https://www.ncbi.nlm.nih.gov/pubmed/23087430 https://web.archive.org/web/20130420211055/http://ncirs.edu.au/immunisation/fact-sheets/hpv-human-papillomavirus-fact-sheet.pdf It's officially summer and that means it's shorts and tank-top season. It also means that you may have noticed some bumps or growths on your child's skin you've never noticed before. Many of these skin lesions can just be left alone and monitored, but some may require that you make an appointment with your child's primary care provider (PCP) to make sure all is well.
If you've recently taken a look at your child's skin and found tiny, skin to pink colored lesions, approximately pinpoint to pencil-eraser in a size, these could be molluscum contagiosum (see here). Molluscum contagiosum sounds scarier than it actually is, but they can become troublesome if not closely monitored. They are warts caused by molluscum virus, which is a poxvirus and causes these annoying non-cancerous lesions. They are painless and spread by direct skin-to-skin contact or by sharing towels with someone who has molluscum contagiosum. The good news is, most times, if left alone, they will resolve on their own. The bad news is that it can take anywhere from 6 months up to 2 years for these pesky little lesions to go away and during that time there is risk of it spreading to other parts of the body, especially if your child has atopic disease like eczema. So what to do? Honestly, less is more. Make sure your child keeps his skin well-moisturized. That way he will be less inclined to scratch at the bumps and spread them to other places. Also, pay attention to where and how many lesions he has. If you start noticing more lesions appearing or if they spread to other parts of the body, you should make an appointment with his PCP for further evaluation. Your PCP can assess the situation and decide whether or not your child can continue to wait it out or if treatment is necessary. While there are many treatment options available, there aren’t any that are approved by the Food and Drug Administration (FDA) for children, and none are guaranteed to speed up resolution. Nonetheless, and depending on the comfort level of your PCP, some treatment options include destruction of molluscum lesions with liquid nitrogen or cantharidin. Liquid nitrogen causes destruction of the lesions by using extremely low temperatures to destroy the tissue at the cellular level. Cantharidin, on the other hand, is a colorless, odorless, terpenoid that is secreted by blister beetles. This causes the skin to blister and in turn, theoretically, destroys the tissue onto which it is applied. Both of these treatments, while effective, can be painful and often leave a pinpoint scar behind after they heal. Other treatment options include application of topical imiquimod or retinoids, oral cimetidine, and Candida antigen injections. If you’ve recently noticed firm, rough, flesh-colored bumps on your child’s body, most often hands or feet, these could be warts. They can also be tan, yellow, grayish, brown or black in color and sometimes they are flat and smooth (see here). Warts are caused by the human papillomavirus (HPV). They are contagious, but more easily acquired with a cut or scrape on your skin. Warts will often go away by themselves without requiring treatment, however, there are some over-the-counter salicylic acid preparations (see here) that are effective and your child’s PCP can treat stubborn ones in the office using liquid nitrogen. In some cases, your child’s PCP may refer you to a dermatologist for reasons such as multiple, recurring warts, if the wart is in sensitive areas such as the face or genitalia, large or painful warts, or if the wart is bothering your child. If you have questions or concerns, just give us a call at ABC Pediatrics. We’d love to see you! Information presented adapted from: https://www.aad.org/public/diseases/contagious-skin-diseases/molluscum-contagiosum https://www.aad.org/public/diseases/contagious-skin-diseases/warts#symptoms https://www.healthychildren.org/English/health-issues/conditions/skin/Pages/Molluscum-Contagiosum.aspx https://www.healthychildren.org/English/health-issues/conditions/skin/Pages/Treatment-For-Warts.aspx http://www.mdedge.com/pediatricnews/article/102139/infectious-diseases/expert-shares-treatment-tips-molluscum-contagiosum Hooray, your child is finally potty trained! You've jumped a big hurdle in parenting. It is no surprise that many parents do a happy dance when their child has learned to use the potty and they can say good-bye to diapers. That all being said, most children will still have accidents from time to time and this is all considered normal. Sometimes there are problems that arise after potty training that may require a visit to your child's primary care provider for further evaluation and management. Keep reading below to find out what some of those problems may be.
One issue parents may encounter during toilet training is bedtime wetting. Now, let me stress that it is not uncommon for children to wet the bed at night during or after potty training. While your child can have bowel and bladder control during the day, it may take longer to achieve bedtime dryness. This usually resolves as the child gets older, which is unique to each child, as he or she will mature at their own pace. As an example, “20% of 5-year-olds, 10% of 7-year-olds, and 5% of 10-year-olds may continue to have bedtime wetting” episodes. The overall idea is that it should happen less frequently as your child gets older. What would be abnormal is if your child has achieved nighttime dryness for > 2 months and then, all of the sudden, he/she starts wetting the bed; or, if your child continues to wet the bed after age 7. There are plethora of possible reasons why this may happen including your child is a deep sleeper and does not awaken when her bladder is full, your child is still learning to hold and excrete urine well, she is constipated thereby putting pressure on her bladder leading to problems with her being able to hold and empty urine effectively, your child may be overly tired, responding to stresses or changes happening at home or she may have a minor illness, family history of wetting the bed (most children who continue to wet the bed have a parent who had the same problem when they were little), her bladder is too small or not fully developed to hold urine for an entire night, and, finally, she may have an underlying medical condition or problem. So what can you do to help your child that wets the bed? Well, first and foremost, don’t blame or punish your child if she wets the bed as it’s not her fault it happened in the first place. Try not to make too big of deal that she wet the bed and reassure her that other kids struggle with it too. Be honest and open with your child letting her know that most kids will outgrow it. It is sometimes helpful to offer rewards for dry nights and offer encouragement and support for wet nights, again no punishment here. Finally, managing bed wetting for your child may even be as simple as making a few changes before bedtime to increase the chance she’ll get through the night without an accident--for example limiting large amounts of fluid about one to two hours before bedtime and making sure your she goes to the bathroom right before bed. If your child is seven years of age or older and is still having bedtime wetting after trying the managing techniques mentioned above for one to three months, it may be helpful trying a bed wetting alarm. We at ABC Pediatrics have found them to be very effective when used correctly. The best alarms are the ones with the sensor that goes directly in the underwear as they detect the instant urine hits the alarm thus waking your child so she can know that she needs to get up and use the bathroom (see here). Now, this will require some work on your part, as you will need to get up at night when the alarm goes off and walk your child to bathroom and reset alarm after. Despite this, we have had good success with our patients who have tried this alarm and many times they will achieve nighttime dryness within a few months. And, if that doesn’t work, and your child is older than 6 years old, there are some medications that can be tried, but often those are not the first-line option and they do have some side-effects. Depending upon the comfort level of your primary care provider, they may refer your child to a pediatric urologist (a doctor who specializes in genitourinary problems) before starting her on medication. Another problem that may arise after toilet training are the occasional daytime wetting accidents. Picture this, your son is watching his favorite show when he comes running to you saying he’s had a “pee” accident. Or, your daughter is running around outside playing with her cousins and you notice that the front side of her pants are all wet. While frustrating for us as parents, these daytime wetting accidents are pretty common. The reason is that toddlers and preschoolers have difficulty sorting and prioritizing the enormous amounts of information and stimuli around them. What seems obvious to us as adults, “I have to go pee, I’ll stop watching my favorite show and do that quickly”, is not so obvious to toddlers and preschoolers. Just be sure that when they do have accidents, you don’t punish them for it, but they should take responsibility for it. What I mean by that is don’t make it too easy on them either. When they have a wetting accident they must stop what they are doing and help you change their clothes, put dirty clothes in laundry, and clean up any other mess, etc. This gives them ownership over the situation and may help them remember that the next time they feel like they have to go potty they will stop what they are doing to go do that because it’s much quicker to go pee in the potty than deal with an accident. While these occasional distracted daytime accidents are normal, what would be abnormal is if your child is complaining of urgency, is frequently having to go pee or is having pain with urination. Sometimes these symptoms can be indications of a urinary tract infection, constipation, or other disease processes. If your child is experiencing the aforementioned symptoms, please call us to schedule an appointment. If your child begins having soiling accidents after she’s been potty trained, that can be a sign of encopresis (fecal incontinence or soling). If your child never fully toilet trains, this is termed primary encopresis, and is a completely different issue. Secondary encopresis, on the other hand, is a result of stool withholding which leads to severe constipation and lessens the child’s ability to hold in her stool ultimately leading to soiling accidents that she may not even be aware of. If this sounds like something your child is experiencing (see here) for more information. It is important you make an appointment for your child with us for further evaluation and management. Well, there you have it. Everything you wanted (or didn’t want to know) about toilet training. I hope this information has been helpful to you and please don’t hesitate to contact us here at ABC Pediatrics with further questions. Information present adapted from: https://www.healthychildren.org/English/ages-stages/toddler/toilet-training/Pages/Bedwetting.aspx https://www.healthychildren.org/English/ages-stages/toddler/toilet-training/Pages/Why-Accidents-Happen.aspx https://www.healthychildren.org/English/health-issues/conditions/emotional-problems/Pages/Soiling-Encopresis.aspx Probably one of the most asked about topics I encounter during toddler well-child examinations relates to potty training. Whether it's recognizing the signs that your child is ready, to which method is the best, to how to actually do it; potty training causes many parents anxiety and undue stress.
Potty training is a momentous milestone in your child's development and as parents, we want it to be a positive one (hooray, no more diapers!). This is precisely the reason why I'm going to take time this month and next month to discuss everything you ever wanted to know about potty training. This month I'll go over the basics and next month I'll dive deeper into common problems that arise after your child has been toilet trained. It is my hope that through these posts, it'll be a positive experience, not only for your child, but you as well. First, and probably most important, is we have to change the way we talk about potty training. The term “potty training” is a misnomer. Here at ABC Pediatrics, we like to think of it more like “potty learning.” Our children are our little apprentices. Like it or not, they learn by watching, listening and the example we set for them. For example, if you don't get excited about vegetables and eat them regularly, would you expect your child do the same? It's the same way with learning to use the potty. Your child needs to see and hear you talk about using the potty before she can be able to do so herself. Think of this like hands-on learning. For the sake of being more simple, I will use the term potty training, but please, think of it more as active potty learning. So how will you know your child is ready? Well, that answer is two-fold. Most children are physiologically ready, that is, their digestive and urinary systems are developed enough that they can hold their urine and stool long enough to make it to a toilet, between 18 and 30 months. That being said, this doesn’t mean that your child is psychologically ready. In other words, at 18 months or 2.5 years of age, your child may not have the mental capacity or desire to be potty trained. Some signs your child may be ready to initiate potty training include: your child begins to demonstrate independence by saying “no,” your child is able to walk and sit down, your child imitates your behavior, your child expresses interest in using the toilet (i.e. wants to flush the toilet, watches you use the bathroom, etc.), your child can tell you when she is peeing or pooping and then begins to tell you that she needs to pee or poop before she is actually doing it, and, finally, your child has the motor skills to pull her clothes up and down or on and off. Physical, emotional, and cognitive readiness happens at different ages for all children, so don't rush it. Just pay attention to these clues that your child may be ready to start the process. There are a plethora of different potty training methods out there and it can be difficult as a parent in deciding which one to implement. Ultimately, the two most common methods in a study conducted by the Agency for Healthcare Research and Quality were the child-oriented approach and the Azrin and Foxx “Toilet Training in Less Than a Day” method, and, both have been found to be effective. The American Academy of Pediatrics (AAP) recommends using a child-oriented approach as it seems to be the most agreeable and reasonable one for most families. This method has parents slowly introduce the potty chair and begin educating their child as soon as she starts showing interest in using the potty. This touches upon what I was discussing earlier regarding how our children learn by watching us. For example, expressing to her when you feel like you have to go the bathroom, letting your child follow you into the bathroom and showing her what you're doing while you're going to the bathroom, have her sit on the potty when you sit on the potty, demonstrating proper wiping technique and subsequently flushing the toilet and then showing her how to wash her hands properly are all ways to begin potty education. Now, if you're like me, the few minutes I use the restroom each day may be the only time I have to myself in a given day. Or, you could be like some fathers I know out there, who are calling the bathroom their new “man cave.” All joking aside, you don't have to take your child on every trip to the bathroom and you'll be surprised how these simple steps spark a whole new interest for your toddler. The biggest take-home point to this child-oriented method is to not push too hard. The key is slow and gentle encouragement. Another common and effective method for potty training that parents have asked me about is the Azrin and Foxx method which uses behavior modification to potty train. Simply put, you pick a day where you don't have to go anywhere, free from other distractions, and you can devote all of your attention to your child, preferably a block of 4 to 6 hours. You then give your child plenty of fluids and snacks and have her sit on the potty regularly with the idea this will help her need to go to bathroom more frequently. Rewards are then given for using the potty and not soiling her underwear and redirection and education if there's an accident. The key to this method is positive reinforcement with successful use of the potty. There is no punishment with accidents. While this method may work for some families, it is not something I typically suggest because it's a very intensive process. That being said, with proper preparation beforehand, it can be very effective (see here). I'd like to leave you with some final tips. Know that with any type of learning, it is a dynamic process and it will likely take some time to master. Setbacks are likely, but with practice, things should improve. Don't be discouraged and remember to stay positive and encourage your child. Once you begin talking about using the potty, bring your child with you to have her pick out a potty. Picking it out herself may give her more motivation to start using it. Also, bringing your child to pick out her underwear can be helpful. I will often recommend parents displaying the underwear in an out-of-reach place as incentive. Your child will likely be excited to put her favorite Disney character or superhero underwear on and will likely not want to dirty them by going to the bathroom in them. Pull-ups are generally unhelpful and should be used sparingly, if at all. They sometimes become a crutch and you don't want the use of a pull-up to give her permission to just pee or poop in the pull-up instead of using the potty. Finally, pick up some of these books from your local library or purchase them for your own library (see here, here and here). They are great introductions for your child and super cute reads. As always, don't hesitate to contact us here at ABC Pediatrics if you have any specific questions or concerns. We'd love to help in any way we can. Happy learning! Information presented adapted from: American Academy of Pediatrics. Toilet training guidelines: Parents -- the Role of the Parents in Toilet Training. http://pediatrics.aappublications.org/content/pediatrics/103/Supplement_3/1362.full.pdf American Academy of Pediatrics. How to Tell When Your Child is Ready. https://www.healthychildren.org/English/ages-stages/toddler/toilet-training/Pages/How-to-Tell-When-Your-Child-is-Ready.aspx American Academy of Pediatrics. Toilet Training 101. http://www.aappublications.org/content/28/5/16 Schmitt, Barton D. Toilet Training: Getting it Right the First Time. http://contemporarypediatrics.modernmedicine.com/contemporary-pediatrics/news/clinical/pediatrics/toilet-training-getting-it-right-first-time#1 As things are beginning to sprout and bloom in Utah, many seasonal allergy sufferers are bracing themselves for the symptoms that often come along each spring. These include runny nose, post-nasal drip, nasal congestion, nasal itching and sneezing. This constellation of symptoms is known as allergic rhinitis in the medical world (I kid you not, I just sneezed while typing this sentence, how’s that for ironic?). If symptoms are mild, they are just annoying, but tolerable. However, if symptoms are severe, they can disrupt daily life and make life miserable. Children, like adults, can also suffer from seasonal allergies. If you suspect this in your child, keep reading along for more information on how to tell if your child may be suffering from seasonal allergies and what you can do to help them.
Allergic rhinitis can be categorized based on the temporal pattern of triggering allergens, the frequency and severity of the aforementioned symptoms. For example, temporal patterns include seasonal (tree or plant pollens at certain times of the year), perennial (year-round allergens such as dust, mold), and episodic (environmental exposures not typically experienced in one’s own home or visiting a home with pets). Frequency of symptoms is divided into intermittent, (< 4 days per week and < 4 weeks per year) and persistent (>4 days per week and > 4 weeks per year). Finally, severity can be categorized by mild (when symptoms do not interfere with activities of daily living) to severe (when symptoms interfere with activities of daily living). So what causes these annoying symptoms of allergic rhinitis? Well, in someone with allergies, whenever his or her body comes into contact with whatever his or her allergic trigger is (pollens, dust, pet dander, etc.), the body releases many compounds, one of which is called histamine. Histamine causes nasal swelling, watery eyes and runny nose. Other symptoms include itchy eyes, nose and mouth and sometimes a rash on the skin (hives). If any of the above sounds familiar, it may be helpful to bring your child into his or her primary care provider (PCP) to be evaluated further. Seeing your child’s PCP is always the first step in managing his or her allergic rhinitis. Most mild to moderate seasonal allergies can be effectively be managed by your child's PCP. At your child’s visit, his or her PCP will get a detailed history and perform a thorough physical examination. If it seems your child is suffering from seasonal allergies, your child's PCP will often begin empiric treatment with an over-the-counter antihistamine. An antihistamine is a medication that blocks that annoying compound your child’s body releases in response to an allergen, histamine. Typically, these medications work well for allergic symptoms, but they may cause drowsiness in some, so often times, your child's PCP will recommend giving it to your child before bed. In addition, he or she will advise your child to avoid known allergic triggers, as that is a huge part in managing allergic symptoms. Finally, depending on the severity of your child’s allergies, or if your child concurrently suffers from asthma, eczema, or food allergies, he or she may refer you to a pediatric allergic specialist for further evaluation, testing and management. The good news is there are ways to treat allergic rhinitis that are safe and effective for children. If you are concerned that your child may have allergic rhinitis or any other allergies for that matter, give your child’s PCP a call to schedule an appointment. As always, don’t hesitate to contact us at ABC Pediatrics for any questions regarding your child’s health. We are happy to help! Please see below for some links for more information on seasonal allergic rhinitis. Information presented adapted from: American College of Allergy, Asthma and Immunology. Seasonal Allergies. http://acaai.org/allergies/seasonal-allergies American Academy of Pediatrics. Allergy Tips. https://www.aap.org/en-us/about-the-aap/aap-press-room/news-features-and-safety-tips/pages/allergy-tips.aspx American Academy of Pediatrics. Diagnosing Allergies. https://www.healthychildren.org/English/health-issues/conditions/allergies-asthma/Pages/Diagnosing-Allergies.aspx American Academy of Otolaryngology Head and Neck Surgery. Clinical Practice Guideline: Allergic Rhinitis. http://journals.sagepub.com/doi/pdf/10.1177/0194599814561600 Our homes are our safe spot, our comfortable place. It's easy to have a false sense of security at home and there may be lurking dangers for your little ones that you are unaware of. It's always a good idea to make sure your house is safe for your little ones. As a pediatric nurse practitioner (PNP), I am not only responsible for caring for children when they are sick, but I am also responsible for promoting the health of children and preventing disease. This includes the prevention of injury as well. This month, I'd like to focus my attention on safety in the home as there have been two, recent, local events of children who experienced preventable accidents while at home.
You may have seen in the news recently a pair of twins who caught national attention after a dresser fell and pinned one of them underneath it (see here). It's a terrifying video for any parent or anyone, for that matter, to watch. Thankfully, neither child was hurt and this brave family has shared their story in order to spread awareness of the dangers of not anchoring unstable furniture. They are especially near and dear to our hearts at ABC Pediatrics because they are our patients (Don't worry, I've received special permission from their mother to share this). It is extremely important to test stability of large furniture pieces: this includes television stands, bookshelves, standing lamps, and dressers. Can they easily tip over if pushed, pulled, or if drawers are opened and climbed on? If so, then they should be anchored to the wall with something like this (see here). Even though I give this advice on a weekly basis, until I saw this story, I had yet to get the dresser and bookshelves in my own two-year-old son's room anchored to the wall. I was aghast to see how easily the dresser tipped over with all the drawers open prior to anchoring. So, thank you Shoff family for the friendly reminder. The next news story, sadly, ended tragically, but it highlights the hidden danger of window-blind cords. This past November, the three-year-old daughter of Reno Mahe, former NFL Eagles player and current running back coach at Brigham Young University, died a week after injuries she sustained from getting tangled in a window-blind cord while at home. Unfortunately, she's not the first child that has died from a window-blind cord strangulation. The U.S. Consumer Product Safety Commission estimates that approximately one child dies each month from window cord strangulation (see here). It is recommended that cordless blinds be used in the home if possible. If those are too cost prohibitive, thoroughly examining all blinds in the home is an absolute must. Be sure to attach the cords for window blinds to wall brackets to keep them well out of reach of children. Any window blind cords with loops should be cut and safety tassels attached as children can be strangled by them if left loose. Anchoring furniture and examining cord blinds are just two home safety items as part of a whole house survey that should be visited every 6 months according to the American Academy of Pediatrics (AAP). The AAP provides a handy check-list that you can take with you and check-off as you go through your house looking for hidden dangers. We provide it as part of our 12-month well-child check packet on our website (see here). It really is amazing how children can turn a seemingly innocent item into something profoundly dangerous. Please make sure to examine your house and do it often. Remember, as your children grow, what once wasn't within their reach, becomes available to them. If you have any questions or concerns, please don't hesitate to contact us at ABC Pediatrics. Information presented adapted from: American Academy of Pediatrics. “Home Safety: Here's How” https://www.healthychildren.org/English/safety-prevention/at-home/Pages/Home-Safety-Heres-How.aspx Cable News Network. “3-year-old Dies After Tragic Window Cord Blind Accident” http://www.cnn.com/2016/12/01/health/elsie-mahe-window-blind-cord-death/ U.S. Consumer Product Safety Commission. “Kids and Cords Don't Mix” https://www.cpsc.gov/s3fs-public/windowcover.pdf I hope you’re having a happy holiday season and that this post finds you well in this last week of 2016. Whether you enjoyed the holidays in the winter wonderland of the Wasatch mountains or lounging in a beach chair near the ocean, I hope you had a joyous holiday weekend. With all that hustle and bustle and being in close quarters with friends and family, you or your children, may have returned home with a little more than some presents. The symptoms of sudden fever, body aches, chills, headache, fatigue, sore throat, cough, and stuffy, runny nose are all characteristics of influenza, more commonly known as the flu. If any of your little-ones are currently experiencing these symptoms, there is a chance they could have the flu. Read on to learn more about what the flu is, how you can help your child get through it, and how you can prevent them from getting it in the first place.
Along with the aforementioned symptoms, children can also experience vomiting and diarrhea while sick with the flu. Furthermore, flu symptoms will typically last one week (7 days) or more. I’m often asked in clinic how parents can know if they or their child has the flu, and my answer is often “Oh, you’ll know.” What do I mean by that? Well, the symptoms of flu are typically much more severe and last longer than a common cold virus. Believe me, if you have ever had the flu, you know you never want to get it again. The flu makes you feel miserable. Your child is also at risk for complications from the flu, like secondary bacterial infections such as an ear infection, sinusitis or pneumonia. If your child is complaining of ear pain, has a lingering cough that’s not getting better, or a fever that persists or suddenly develops again after not having one, you should take your child to see their primary care provider (PCP). Influenza is caused by a respiratory virus that is spread via droplets in the air or by touching infected surfaces and then touching your nose, eyes or mouth. For example, if someone with the flu sneezes, virus particles are released into the air, and if your child happens to be nearby and inhales those particles, he now has a chance of coming down with flu. Similarly, if someone with the flu sneezes into their hands and then touches a door handle to open a door and then your child touches that same door handle and then rubs his eyes, he could come down with the flu. The flu virus is most contagiousness in the first few days of the illness, but it can be spread a day before symptoms start and up to a week or more after symptoms began. This is another reason to keep your children home when they are sick, so as to not spread disease. The flu is treated with supportive care; lots of rest, lots of fluids, and lots of love. If your child seems like they are in pain or uncomfortable from the fever or other flu symptoms they are experiencing, you may give a pain or fever reducing medicine such as Acetaminophen. Make sure to use the correct dose for you child’s current weight (see here). Because the flu is caused by a virus, antibiotics are not helpful. However, if your child has a chronic health problem like asthma, diabetes, sickle cell disease, a chronic neurological condition then he or she may benefit from an antiviral medication that is only available by prescription from his or her PCP. Antiviral medications are most effective at reducing influenza severity and illness duration if start within forty-eight hours of symptom onset. The single best way to prevent your child from getting the flu is to have him or her vaccinated against the flu each year. The American Academy of Pediatrics (AAP), recommends that an influenza vaccine be given each year to all children beginning at six months of age. Children 6 months through 8 years of age may need two doses given at least four weeks apart if they’ve never received 2 in one season. Children ages 9 and older only need one dose. In addition, it is also recommended that anyone who will be in close contact with your child or any other caretakers receive an annual flu shot as well. This is especially important if your child is not old enough to receive a flu shot. The flu shot is safe and effective and has few side effects, if any. The most common are local injection site redness, soreness, or swelling, and fever. In Utah and the surrounding Intermountain West the best time to get your child his or her flu shot is October through November – sooner if your child has a chronic illness that may make the consequences of an influenza infection more severe (see conditions listed above). That being said, if you haven’t had a chance to get your child vaccinated yet this season, it’s not too late. Go get them vaccinated as soon as possible. Finally, practicing good hand hygiene, eating a nutritious diet, and getting adequate rest are all great ways to prevent your children from getting sick. Please, if you have any questions or concerns about what was discussed in this month's post, don't hesitate to contact us here at ABC pediatrics. We are happy to answer any questions you might have. Wishing you and yours a very happy and healthy 2017! Information presented adapted from: American Academy of Pediatrics, Recommendations for Prevention and Control of Influenza in Children, 2016-2017 http://pediatrics.aappublications.org/content/early/2016/09/01/peds.2016-2527 American Academy of Pediatrics, The Flu https://www.healthychildren.org/English/health-issues/conditions/chest-lungs/Pages/The-Flu.aspx Centers for Disease Control and Prevention, How Flu Spreads https://www.cdc.gov/flu/about/disease/spread.htm Just when you thought you wouldn't survive the “terrible twos,” there is yet another age to fear during your child's growth and development and that's the year of the “threenager.” What is a threenager you ask? If you do a basic search on the web, you can get a variety of equally funny, yet terrifying answers (this was my personal favorite). Most suggest that a threenager is a three year old that acts and has the attitude of a teenager. In case you're not parenting a teenager at the moment or you've forgotten what it's like to be one, let me refresh your memory. Think: mood swings, emotional outbursts out of nowhere, angst, and fighting for independence, but all the while still needing mom and dad. All joking aside, my hope is to explain what your three-year-old child is going through and why many of her actions are developmentally appropriate. Maybe that will ease some of the frustration and the “I’m going to pull out my hair if she refuses to put on her pants one more time!” moments. I also hope that I am able to give you some tools on how to better parent your threenager so you are more prepared once they become actual teenagers!
To understand why your once darling child is behaving like a megalomaniac it first helps to explain what’s going on in her brain. Dr. Daniel Siegel, a child and adolescent psychiatrist, and Tina Bryson, Ph.D., a pediatric and adolescent psychotherapist, break down brain development quite well in their book, “The Whole-Brain Child.” Our brains are divided into two hemispheres, the left and the right. Our left brain is logical; our rational, literal, linguistic and linear centered thinking occurs here. Conversely, our right brain is more emotional; It is non-verbal and holistic. It sees the entire picture and the feelings that go along with it. From a developmental standpoint, toddlers--children ages one to three--are right-brain dominant. That means they have not yet developed a logical way of thinking. Therefore, they are living “emotionally” and cannot use words or logic to describe their feelings and live completely in the here and now. Have you ever wondered how your child has the uncanny ability to drop everything she’s doing to gaze at every rock or animal on the way to get in the car to drive to school, not caring that you clearly have some place to be? It’s not that she’s trying to drive you crazy, it’s that she has no sense of time and can’t rationalize that getting to school on time is more important than staring at rocks and cute animals. Is this sounding familiar? That being said, when your child finally begins to ask the dreaded “why?” use that as a clue that her left brain is emerging. The reason she wants to know why you have to get in the car, and why she must get in her car-seat and why she needs to go to school is that her left brain, that part of our brain that likes to know the cause and effect of relationships, is waking up. Furthermore, your child wants to be able to verbalize those rational thoughts with language. In addition to right and left-brain dominance, the prefrontal cortex (the part of the brain that provides behavior regulation and carries out executive function) is also still developing and will continue to mature through adolescence and into early adulthood. In other words, this is the part of the brain that helps differentiate among conflicting thoughts, good and bad, better and best, same and different, and performs social “control.” So, the reason your child unexpectedly lashes out at you because you (heaven forbid) cut her grilled cheese in half is because that part of her brain has not fully developed yet. It’s going to take some time for her to be able to self-regulate and control these emotions. At three years of age, your child is officially out of the toddler stage and into the preschool stage. Socially and emotionally she likes to imitate adults and friends. She is beginning to show affection for friends without being prompted. She displays a wide variety of emotions (sometimes to your dismay!) and may get upset by changes in her routine. She begins to engage in fantasy play and she may have a difficult time telling the difference between what’s real and what’s not. As far as language development goes, she can speak in sentences of five to six words and speaks clearly enough for most strangers to understand. She may begin to tell stories and she has mastered some basic grammar rules. Cognitively, she can name some colors, she can count and may know a few numbers. While most toddlers have no concept of time, three-year-olds are starting to have a clearer sense of it. She can follow three step commands (when she wants to) and she now understands the concepts of “same” and “different”. In a nutshell, your threenager is practicing her independence. She wants to make her own decisions and feel like she’s in control, but she also needs you, her parents, as well. Tovah Klein, Ph.D., professor of psychology and director of the Barnard Center for Toddler Development in Manhattan, as well as the author of “How Toddlers Thrive” writes that children this age have primary needs that are motivated by two instinctual drives “the need to separate and the accompanying desire to become an independent being with a sense of self.” Even though she wants to begin to separate from you, she also wants to know you’re still there to set limits, provide comfort, guidance, and protection. It’s what she calls the “toddler paradox,” they push us away, only to pull us close again. All of this right brain dominance with left brain emerging, lack of self-regulation, wanting control, push and pull, can make the task of parenting very challenging for us parents. Fortunately, instituting a few the following tips can make life a little easier (see here for entire list). While I don't have the time to discuss all of these tips, there are two I'd like to highlight. One is to be attuned to your child. This may be one of the most important tips because when we are seeing the world through our child's point of view we can better understand why the melt-downs take place. For example, let's say your child throws a fit each time you try to put her coat on her while you're trying to get out the door in the morning. The morning rush can be difficult for three-year-olds and for parents alike. It's often hurried and your child's needs or wants may be overlooked in the chaos. Being attuned means figuring out why she doesn't want to put on her coat in the first place. When you take the time to slow down and ask her, you find that she doesn't want to wear the pink coat, she wants to wear the blue coat. Aha, problem solved! Another important tip I'd like to discuss is to be consistent. This means that, as a parent, you consistently address behaviors that are problems. Three-year-olds need this consistency. They want to know what to expect in a given situation, but it is also natural for them to test their limits. For example, if you don't want your child to play with her food at the table today, you act on it right now, and then again tomorrow and the next day if she does it. Calmly say “Please don't play with your food. You can either eat in the chair or play on the floor, but you can't play with your food at the table”. If she begins to play with her food, you gently and calmly take away her food, take her out of her highchair and place her on the ground. What you've done here is given her a choice, which she made, and now come the consequences of that choice. This needs to consistently happen for the misbehavior to be replaced with good behavior. Also, make sure that other caregivers are on the same page as well. Finally, please don't forget that for each time you correct your child, you should be offering praise or loving words ten times more and praise effort, not the outcome. This way she gets positive attention and not negative attention. Now that you are equipped with the knowledge of your three-year-old's current developmental state, coupled with some tips to help you parent her, you will survive the year of the threenager. Think of this year as being Mother Nature's way of helping you survive the teenage years. Good luck! Information presented adapted from: American Academy of Pediatrics, Tips to Survive the Terrible 3s. https://www.healthychildren.org/English/ages-stages/preschool/Pages/Tips-to-Survive-the-Terrible-3s.aspx American Academy of Pediatrics, Developmental Milestones 3 to 4 Year Olds. https://www.healthychildren.org/English/ages-stages/preschool/Pages/Developmental-Milestones-3-to-4-Year-Olds.aspx Klein, Tovah, How Toddlers Thrive https://www.amazon.com/How-Toddlers-Thrive-Children-Lifelong-ebook/dp/B00DPM7V20 Siegel, Daniel J & Bryson, Tina P, The Whole-Brain Child https://www.amazon.com/Whole-Brain-Child-Revolutionary-Strategies-Developing/dp/1491514817 In last month’s post I shed a little light on infant sleep patterns (see post). This month, I will try to do the same by discussing common sleep problems in the toddler years and beyond. I have organized this month’s post into a question and answer format as I did in last month’s post, based on similar questions I’ve received in clinic. Please don’t take the following advice as “the end all be all.” What works for one child, doesn’t always work for another. However, I have found many of these suggestions to be helpful to my patients and their families and personally as a mother myself.
1) We recently moved our 3-year-old son to a toddler bed to prepare for his baby sister’s arrival in a few months. Prior to this, we had no trouble putting him to sleep in his crib. Now, bedtime is a struggle and we cannot seem to get him to stay in bed. As soon as we put him down for the night, he either calls out crying for us to come into his room or he just gets up out of bed. Sometimes this happens multiple times a night. How can we get him to stop this behavior? Answer: It is normal for children of this age to resist going to sleep, especially if they have older siblings that are still awake. First, it is important to have a bedtime routine in place and that you are consistent with it. For example, I often suggest that the hour before bed be designated “quiet” time. This means no stimulating activities about an hour before bed. This is true for all age groups. This includes TV, video games, electronic toys, and active play. All of these activities could make your child too excited to sleep. It is also helpful to use this time to carry out a bedtime routine--taking a bath, brushing teeth, listening to quiet music or reading a story, and then going to bed. It is also helpful to have your child take a favorite thing to bed each night like a teddy bear or blanket and to make sure he or she is comfortable. By addressing your child’s needs (a drink of water, using the bathroom or leaving the door open a crack to let a little light in the room) before bedtime this will hopefully make it less likely that he or she will feel the need to use them as excuses to avoid going to sleep later. The preschool age group (children ages three to five) is also a time when I like to discuss the idea of a “bedtime pass”, especially for parents who are at their wits end. The bedtime pass is basically a 5 x 7 index card that you give to your child explaining that the pass is good for one bedroom exit per night. That could be anything, an extra hug and a kiss, a trip to the bathroom, or a drink of water. After the pass has been used for one choice off the list each night, your child is not allowed to leave his or her bedroom or call out for you as the pass has been used. The idea is that, over time, your child won’t want to use up their one pass at night because they want to be able to use it when they REALLY need it and the night time “calling outs” and getting up out of bed will happen less and less until they become non-existent. The bedtime pass also makes a highly stress-ridden situation less emotional and more transactional, giving both the parent and child control in the matter. It ends up being a win win. 2) My 2-year-old daughter has been waking up screaming in the middle of the night. When I go to check on her, she looks like she's still sleeping, but it sounds terrible. Is there anything I can do to help this? Answer: Night terrors are particularly distressing for parents. They occur most often in toddlers and preschoolers and take place during your child's deepest stages of sleep. Some signs of night terrors are crying uncontrollably, sweating, shaking, or breathing quickly. Your child might have a glassy-eyed gaze, a terrified or confused look on his or her face. He or she may thrash around in bed, scream, or kick. Your child may not recognize you or realize you are there and they may push you away if you tried to hold him or her. Night terrors can last anywhere from seconds to minutes, sometimes up to 45 minutes. Most children will fall back to sleep immediately following a night terror because they actually haven't been awake. Also, most children don't end up remembering night terrors and will have no recollection of the events of the previous night the next morning. Night terrors are often an inherited disorder, meaning parents of children with night terrors often suffered from night terrors themselves. They also are a product of sleep debt or being overtired, meaning your child likely hasn't been getting enough sleep recently. So what can you do? If your child is having a night terror make sure that you relax, as again, they are usually more frightful for you than for your child. Don't try to wake him or her. And, keep your child safe. If your child tries to get out of bed, gently restrain him or her. Finally, the best way to prevent night terrors from happening in the first place is to make sure your child is getting enough sleep. For example, if your child's current bedtime is 8 pm, try putting him or her down about half an hour earlier, so 7:30 pm and see if that helps. Many times, parents can recall a week of late bedtimes or not good sleeping as the culprit and once back into a good routine, they happen less or not at all. 3) My 5-year-old son is constantly bouncing off the walls. He has trouble focusing during the day, sitting still, and is quick to act out. He will often lose his temper and lash out at his younger siblings too. He seems to be doing fine in school, but I worry that these might be the beginning signs of ADHD? What should I do? Answer: While these can all be signs of a child with ADHD (see this post for more information on ADHD), what is more likely, given his age, is he’s not getting enough sleep. There exists a lot in the scientific literature that shows getting less the recommended amount of hours of sleep each night leads to attention, behavior and learning problems in children. In addition, in a child with ADHD, poor sleep can make these condition even worse. However, as a clinician in this scenario, it is important to make sure that this child is getting adequate sleep before jumping to any conclusions. According to the American Academy of Sleep Medicine, there are an average number of hours of sleep per night your child should be getting for optimal health and functioning. The amount of hours differs depending on the age of your child and it decreases as your child grows, but it is probably more than you think it is (see here). Some of my first questions to this parent would be what time is bedtime, what does your child do in the hour leading up to bedtime, and do you have a nightly routine? More often than not, we find that the hyperactivity and temperament of the child is due to a late bedtime or poor sleep pattern more than ADHD or any other medical diagnosis. 4) Help! I feel like I always have to drag my 15-year-old daughter out of bed in the morning. She says she “just can’t fall asleep at night.” She is in bed at 10 pm most nights, but says she lies in bed, tossing and turning for hours each night. Should I start her on a sleep medication? Answer: Before starting your daughter on any kind sleep aid medication, it is important to first make sure she doesn’t have any bad bedtime habits that are making it difficult for her to fall asleep. We live in a technological age and that has made falling asleep more difficult for many people. So what to do in this situation? First, make sure your daughter avoids any kind of screen time one hour or more before bedtime. That means no cell phone, computer, tablet, TV screen, etc. Basically, "if it lights up it’s off limits." Many of my teenage patients are aghast when I suggest this. They tell me “How will I get up in the morning? My cell phone is my alarm clock.” I think they are even more surprised to realize there were and still are these things called alarm clocks that ring and they can be used instead of their cell phones to wake up in the morning. Now, I know sometimes this rule isn’t always realistic because homework sometimes needs to be completed on a computer and it can’t always be started by a certain time with activities and/or sports in the mix. However, if for the most part, this rule and bedtime is respected, falling asleep will become easier. Second, no electronics are to be allowed in her bedroom. For example, if her phone is on silent or sleep mode, her brain still knows the phone is in the room and she could be tempted to look at it and see who texted her. By not allowing electronics in the bedroom, it is used only for sleeping and her body will know that too. Many parents will have their kids “turn in” their cell phones for the night after a certain hour which helps carry out this idea. Finally, as mentioned in the first question above, a nighttime routine is helpful for good sleep hygiene. A ritual of quiet time, taking a shower or bath, brushing teeth and reading before bed, can help settle down the brain at night. Hopefully, by making these simple changes, your teenager will be falling asleep easier in no time. It is my hope that you found some applicable solutions to sleep challenges your family is facing at the moment. If you have more specific questions, or any question for that matter, please don’t hesitate to contact us here at ABC Pediatrics. Sweet dreams! Information presented adapted from: American Academy of Pediatrics, Bedtime Trouble. https://www.healthychildren.org/English/healthyliving/sleep/Pages/Bedtime-Trouble.aspx American Academy of Pediatrics, Sleep Problems. http://www.pediatricspec.com/resources/SleepProblems.pdf American Academy of Pediatrics, AAP endorses new recommendations on sleep time. http://www.aappublications.org/news/2016/06/13/Sleep061316 Clark, Wendy Mitman, The Bedtime Pass Help Parents And Kids Skip the Sleep Struggles. http://www.npr.org/sections/health-shots/2015/09/18/441492810/the-bedtime-pass-helps-parents-and-kids-skip-the-sleep-struggles Sleep. Everyone needs it. We don't get enough of it. Most people wish they got more of it. Whether it’s tired parents of newborns who are up every few hours in the middle of the night to feed their baby, frustrated parents of toddlers who won't stay in their beds, or exasperated parents of teenagers whose children won’t get out of bed because he or she stayed up until midnight binge-watching Netflix, parents are concerned about their child’s sleeping habits and with good reason. No matter the age, sleep is extremely important to our overall health and well-being. A well-rested body and mind is a well-functioning body and mind. While I can't make your child sleep, I can try to give you suggestions to foster a positive environment for sleeping and prevent bad habits from taking root, no matter what stage of life your child is in. Because sleep is such a broad topic, I've broken it up into 2 parts. This month, I'll discuss sleep in infancy, that is, newborn to 1 year of age, and next month I'll tackle some sleep issues for toddler years and beyond. I've organized this month's post in a question/answer format. These are similar questions to those I have received at clinic regarding infant sleep.
1) How much sleep should my baby be getting everyday? Answer: It depends on how old your baby is. Newborn sleep patterns differ greatly from the sleep patterns of older children and adults for they will not develop a regular sleep pattern until about 6 months of age. Newborns up until 6 months of age need a total of about 16 to 18 hours of sleep daily. In the newborn period, this sleep is broken up into increments and babies will wake every 2 to 3 hours to eat and then fall back asleep again sleeping only 1 to 2 hours at a time, with some periods of wakefulness. At about 2 months of age, infants will start stretching out their sleep with a preference for sleeping at night, about 5 to 6 hours at a time, and then are awake for longer periods during the day. By 6 months of age, many babies are sleeping at least 10 hours at night with 2 to 3 naps during the day. This longer stretch of sleep at night is again mirroring the sleep patterns of older children and adults. By one year of age, most babies are sleeping 11-12 hours at night and have 1 to 2 naps during the day. 2) When can I expect that my baby will be sleeping through the night? Answer: Sleeping through the night during the first few months of life means a baby is sleeping about 5 to 6 hours at night without needing to eat. This usually happens around 2 months of age, although some babies begin earlier. Most parents of newborns will agree, that first time your baby gives you a 5 to 6 hour stretch of sleep, you feel like a new person, especially if it continues. As your infant grows, that stretch of sleep will increase, and your baby will baby able to go for longer stretches of time without eating. 3) Why isn't my son a good sleeper like his cousin? My son is 2 months old and his cousin who is the same age sleeps 10 hours a night without waking up. What am I doing wrong? Answer: First, let me describe what a good sleeper is at 2 months of age. A good sleeper is a baby that sleeps at least 5 to 6 hours at night and during those long stretches may wake up every so often, but can put himself back to sleep. I would be concerned if the parents of a 2 month old told me that their baby slept 10 hours a night without waking. It is developmentally appropriate for a child to wake often, as this shows the infant can wake in situations where they're not getting enough oxygen or if they are having trouble breathing. Because infants wake often in their sleep, this is another reason why it's important to not always rush and get them out of bed at each little cry. I call this the “declaration period”. Let your baby “declare” himself awake. In France, they call this “Le pause”. Many times babies cry out as they are transitioning from one sleep cycle to the next. Give it a few minutes and see if he can soothe himself on his own and fall back to sleep before taking action. If he is still crying after 2 to 3 minutes, go check on him. 4) My daughter is 3 months old and needs me to rock her to sleep. How can I get her to fall asleep on her own? Answer: The trick to getting her to sleep on her own is putting her to bed when she’s drowsy, but not asleep. For example: if she needs you to rock her to sleep to put her down at night, then anytime she gets up in the middle of the night she will likely need you to rock her to put her back to sleep. This then creates a vicious cycle. Pay attention to signs that she’s getting sleepy, this might include her yawning or rubbing her eyes, but be sure to not wait too long until she’s over-tired, as that makes getting her to sleep on her own even more difficult. Don’t worry, as time goes by, you’ll get to know your baby’s tired cues and by putting her down as the first signs of sleepiness and she will learn to settle herself to sleep. Another good habit to develop is a bedtime routine. You can even begin this when your baby is still on the every 2 to 3 hour feeding schedule. Early on, this is teaching your little one that nighttime is for sleeping and daytime is for playing. Also, a bedtime routine creates consistency and consistency is key in parenting. By performing the same ritual each night, babies will come to know it’s bedtime and, therefore, will have an easier time falling asleep. This bedtime routine could be as simple as making sure lights are turned down low about an hour before bed, giving a bath, doing the final feeding of the night, reading a book and putting your child to bed while drowsy, but not asleep. Finally, always be sure you’re putting your infant on his or her back to sleep. The best sleep is safe sleep, so remember Back to Sleep! 5) Help! My 6 month old son still wakes up every 2-3 hours in the middle of the night to nurse? He acts so hungry and then immediately goes back to sleep when he’s done. I’m so tired though, I can’t go on like this. Answer: One common phrase I often hear from parents of older infants who aren’t sleeping through the night is “He must wake up because he’s hungry because once he eats he goes right back to sleep”. And, while this seems logical, this is one of those instances where he’s likely gotten in the habit of snacking in the middle of the night and this is not a necessary feeding. A healthy, thriving 6 month old does not need to eat in the middle of the night. I will often say to parents “Well, if you offered me chocolate chip cookie, I’d eat it too”. So, what to do now? Well, we have to rid him of this bad habit. The best way to do this is still quite the debate and many people feel strongly that some ways are better than others. There are a plethora of different methods (extinction i.e. “cry it out”, graduated extinction, bedtime fading, scheduled awakenings) and the good news is, no matter what method you choose they work. A recent New York Times article highlighted a systematic study that was published in 2006 in the journal of Sleep on the efficacy on these interventions. After reviewing fifty-two studies, 94 percent of those reviewed reported improved sleep with implementation of any studied intervention. Hooray, there is hope! What I would recommend in the case of this 6 month old that is nursing every 2 to 3 hours is the extinction method with some slight modifications. The extinction method has parents let their infants “cry it out”. After performing a nightly bedtime routine, parents do not go in the room until morning. Now the traditionalists of this method would say to not go in the room, under any circumstances. That may be quite harsh for some parents (It was for me!). What I have parents do is set a timer, usually 10 minutes. If after 10 minutes, he is still crying (which he likely will be) it is okay to go in his room and make sure he’s okay. If all is well, and he’s just upset that he’s not getting his 1 am snack, you tell him you love him, that he’s safe and he needs his sleep just like mommy and daddy do. This is another French parenting tip – talk to your babies. The French believe babies understand what you’re saying (as do I) and it makes you feel better too. The first night of this method will be brutal, but it will get better. If he cries on and off the first night for 3 hours, by night two it may only be 45 minutes, and by night three it may be only 30 minutes, and most often, by 1 week, they are sleeping through the night. I’m not going to lie, there is nothing easy about listening to your baby cry, but you have to keep the end goal in mind and that is, a night of good sleep, for your child and for you. You will sleep again, I promise. I won’t ever forget that one of the most helpful words of encouragement I received in the first few weeks after becoming a parent myself was “I know you are tired right now, try not to worry, you will sleep again”. During that time, with sleep deprivation weighing heavy, to hear that sleep deprivation was only temporary was a tremendous relief. It is my hope that whatever sleep struggles you are experiencing at the moment you'll find some guidance and comfort in reading this post today. As always, if you have a more specific sleep concern or any other questions, please don’t hesitate to contact at ABC Pediatrics. We are here for you! Information presented adapted from: American Academy of Pediatrics, Sleep: What Every Parent Needs to Know. http://shop.aap.org/Sleep-What-Every-Parent-Needs-to-Know-Paperback/ American Academy of Pediatrics, Sleep Problems in Children. http://www.pediatricspec.com/resources/SleepProblems.pdf Carroll, Aaron, Putting Your Baby to Sleep: Some Advice and Good News http://www.nytimes.com/2016/08/02/upshot/putting-your-baby-to-sleep-some-advice-and-good-news.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0 Druckerman, Pamela, Bringing Up Bebe https://www.amazon.com/Bringing-Up-B%C3%A9b%C3%A9-Discovers-Parenting/dp/0143122967 So, I’m just going to get straight to the point. Concussions scare me. Anything that involves injury to one of our most vital organs makes me uncomfortable and is never something I want any of my patients to experience. What is even scarier to me is that I’ve found many have a nonchalant attitude towards this issue or don’t know much about it at all. A concussion is not something to mess around with. It can cause long-term consequences if not handled appropriately. Here’s what you need to know as parents:
According to 3 international symposia on concussion in sport (CIS), a concussion is a mild traumatic injury to the brain and can be caused by either a direct blow to the head or somewhere else on the body with enough force transmitted to the head. There are various ways one can sustain a concussion, such as playing football or soccer when two players collide and hit heads, or while recreating, like riding a bicycle and falling off and head meeting the ground. One could even be so unlucky to just slip on a patch of ice and smack their head on the ground. Now, typically, there will be some kind of immediate neurological impairment that will go on to resolve spontaneously, with or without a loss of consciousness. However, sometimes, signs and symptoms may not appear for minutes to hours after the blow initially occurred. A graded set of clinical symptoms will result from a concussion and resolution of these clinical and cognitive symptoms will often follow a set course. These symptoms fall into 4 categories: physical, cognitive, emotional and sleep. Physical signs include headache, nausea, vomiting, balance issues, visual changes, fatigue, light sensitivity, noise sensitivity and an overall dazed and stunned feeling. Some cognitive signs commonly experienced include trouble concentrating and impaired memory. Patients experiencing head injuries often have difficulty controlling emotions. They become easily angered or move from one emotion to another quickly. Sleep is often confused, with patients either experiencing more lethargy or conversely, trouble falling and staying asleep. Increased or prolonged drowsiness is a concerning finding in these patients as well. If you think your child has sustained a concussion, he or she should be evaluated by a healthcare professional as soon as possible. Once evaluated, your child’s health care provider will determine if head imaging is warranted (in most cases it’s not). If all looks well and concussion is the diagnosis, your child’s health care provider will spend some time explaining activities and situations to avoid during a period of cognitive and physical rest. Cognitive rest could be anything from shortened days at school, to a temporary leave of absence from school, to a reduction in school workload or more time given to finish homework or exams. Video games, using a computer or tablet, and watching television should also be discouraged during this time as these require concentration and attention and can worsen symptoms. In addition to cognitive rest, children who have suffered a concussion should be withheld from any kind of physical exertion until they are symptom free while at rest. This definition is broad and not only includes sports or the activity that caused the concussion in the first place, but other leisure activities that causes physical exertion, such as biking, skating, swimming, and jumping on trampolines, just to name a few. Once your child is feeling symptom free at rest and would like to start participating in sports or other physical activities, a graded return-to-play progression is recommended (see here). Each step should be given 24 hours, and should take your child a minimum of 5 days to complete the protocol in order to get back to no limitation in activity. All of this is dependent on no symptoms returning. If there are any problems or if symptoms return while going through protocol, your child should stop that activity immediately. Once he or she is asymptomatic after another 24 hours of rest, your child should go back to the previous asymptomatic level completed and go on from there. Make sure to contact his or her health care provider if symptoms recur as well. Now the big question is how long should your child undergo physical and cognitive rest and when should the symptoms resolve? The truth is, there is no set time. Most symptoms will resolve within 1 week and some take up to 2 weeks or more. If your child’s symptoms don’t resolve within 2 weeks, he or she could be suffering from post-concussive syndrome, which basically means they're experiencing 2 to 3 of those symptoms mentioned above for longer than 2 weeks. Again, not much can be done to help expedite the process except for giving them more time to recover. Making sure your child is symptom free before getting back to activities, especially contact sports, is the most important piece I want you take home from this post. Please, DO NOT let your child get back in that game or back on that bike or skateboard, until they are completely symptom free. So many times in clinic I've heard “But he has a big tournament this weekend” or “She will be heart broken if she can't play”. While I sympathize I can't stress enough the grave danger in sustaining a second concussion before symptoms of the first have resolved. It is called second-impact syndrome, and it can cause swelling in the brain that can lead to death. All reported cases of second-impact syndrome have been in patients less than 20 years of age. While extremely uncommon, it can happen. There is much truth to the saying “when in doubt, sit them out”. It's just not worth it. Finally, is there a certain point to retire your child from one or multiple sports for the risk of getting another concussion? For example, what if your child had a concussion 1 year ago while playing hockey and just took a big spill off their mountain bike and suffered another 1? Unfortunately, there are no evidence-based guidelines that definitively give a number. It has been proposed that 3 concussions in one season or post-concussive symptoms that last greater than 3 months should warrant further conversation between you, your child, and his or her health provider regarding an extended time away from sports. As hard as of decision that may be, your child's safety and well-being are most important. While we can't prevent all concussions from happening, the wearing of protective gear, identifying at risk athletes, and providing education regarding the dangers of concussions are the most important aspects of protecting our children. Information presented adapted from: American Academy of Pediatrics, Sport-Related Concussion in Children and Adolescents, http://pediatrics.aappublications.org/content/126/3/597 McCrory P, Meeuwisse WH, Aubry M, et al., Consensus statement on Concussion in Sport, http://bjsm.bmj.com/content/47/5/250.full.pdf+html In last month's post, I discussed ways to keep your kids safe in the sun and water never thinking I'd have to practice what I preach. Let me share a recent experience I had with my little guy a few weeks ago. At a family BBQ, I was instituting “touch supervision” with my water-obsessed toddler. I'm not exaggerating. You know how they say “where there's a will, there's a way?”. Well, “where there's water, there's my Joe!” Anyway, I digress. So, at this BBQ, I was exhaustively keeping up with him as he went in and out of a kiddie pool and was running around the yard. At one point, while chatting with a friend, I took my eyes off off him for just a second, and sure enough, he went head first, feet flailing up in the air into a melting bucket of ice that was holding all the beverages. Fortunately, because I was right next to him, I pulled him out just as quickly as he went in. Aside from being stunned and coughing from swallowing some water, he was fine. However, the entire incident hit home...hard. If I hadn't been paying attention, this could have played out much differently. It was a lesson for me, and I hope for anyone reading this, how important it is to not let our guard down. In this season of endless fun and outdoor activities, it's important to be aware of the possible dangers as well--that way we can all have a happy, healthy and safe summer. Now on to this month's post: bicycle, firework, playground and lawn-mower safety.
I think most of us remember the first time we rode a bike, especially without any training wheels. It is often a developmental milestone most of us remember fondly, that is, if all ended well. As parents, we need to think of a bicycle as our son's or daughter's first vehicle. Riding a bike offers a new found freedom and endless hours of fun, but it is also important to be aware of the risks. First, and probably most important, if your child is on a bike, or any other moving object for that matter (i.e. scooter, skate board, roller-skates, etc) they should be wearing a helmet. I think there is a misconception that if they are just riding in the driveway or not going far away from home, they don't need to wear a helmet, but most accidents happen close to home. In fact, here at ABC Pediatrics, we know of children who have suffered traumatic brain injuries (TBI) in their own driveway from a fall off a bike. Helmets should be worn at all times. Make sure the helmet fits properly so that it covers the forehead and does not tip forward or backward. The strap should be secure enough that you can fit only 2 fingers between your child's chin and the strap. The helmet should feel snug, but not overly tight. Also, when choosing a helmet, make sure there is a label verifying it meets the Consumer Product Safety Commission's (CPSC) safety standards. Having trouble getting your little guy to wear his helmet? Well, just as I mentioned in last month's post, children learn best by observing you. If you want your child to wear a helmet, it is best that you wear one too. Also, don't let them have an option of wearing one. They either wear a helmet or don't get to ride their bike. Other bicycle safety tips include, picking an appropriate sized bike based on child's developmental age and height. For example, don't take those training wheels off until your child is good and ready. Also, teach your child to ride on the right hand side of the road going along the direction of traffic, use hand signals, and obey traffic signals and all signs. With the long, holiday weekend approaching, it's the perfect time to discuss firework safety. While the fireworks of the Fourth of July are beautiful and fun to watch, fireworks can cause severe injury, even death. Fireworks that are traditionally thought to be safe for children, like sparklers, can cause severe burns to both the person handling them and others around them. According to the United States (U.S). Consumer Product Safety Commission, firework related injuries accounted for an estimated 10,500 emergency room visits in the US in 2014. Moreover, children younger than 15 years of age accounted for an estimated 35 percent of those injuries. Given this information, let's leave the fireworks to the professionals and attend community firework displays, rather than using them at home. Children using playground equipment should be supervised by an adult at all times, whether at home or at a park. Prior to letting your child play on playground equipment, inspect it for loose nuts or bolts or open “S” hooks as those can harm children. Playground equipment should have safety-tested mats or loose fill materials, like wood chips, and be maintained at a depth of 9 inches with at least a 6 foot surround, especially for swings and slides. Playground equipment made of metal, plastic and rubber can over heat in summer time, especially when it is sunny outside, so double check that it's not hot. Make sure that children aren't wearing lose clothing and that helmets are taken off prior to using playground equipment. The ownership or use of home trampolines is not recommended by the AAP as there is a serious risk for injury, even when children are being supervised. Some trampolines have a netting surrounding a trampoline, but this too often provides parents (and children) with a false sense of security. Most trampoline related injuries happen while actually jumping on the trampoline itself, not from falling off of it. If a child does play on a trampoline, he or she should be supervised at all times and only one person should be jumping at a time. Just this week there was a great article in The Wall Street Journal that discussed the danger lawn-mowers can pose to children. According to a new study from University of Tennessee in Memphis, over 9,000 children are injured each year while mowing the lawn. Now, this doesn't mean your child shouldn't mow the lawn or perform other chores (sorry kids!). All this means is they should be of an appropriate age and follow some simple steps to prevent injury. The AAP recommends that a child be at least 12 years old before using a walk-behind mower or hand mower in order to use it safely and they also recommend that a child be at least 16 years old before they can use a riding lawn-mower safely. Make sure you teach him or her how use the lawn-mower properly and supervise them until they can manage to complete the task independently. Click here for additional safety tips before, during and after mowing the lawn. Well, that's a wrap. That was a lot of information. As always, if you have any specific questions, don't hesitate to contact us here at ABC Pediatrics. Enjoy the rest of your summer and have a wonderful and safe Fourth of July weekend! *Information presented adapted from: American Academy of Pediatrics, HealthyChildren.org, “Bicycle Safety: Myths and Facts” https://www.healthychildren.org/English/safety-prevention/at-play/Pages/Bicycle-Safety-Myths-And-Facts.aspx American Academy of Pediatrics news feature “2016 Summer Safety Tips” https://www.aap.org/en-us/about-the-aap/aap-press-room/news-features-and-safety-tips/pages/Summer-Safety-Tips.aspx?nfstatus=401&nfstatus=401&nftoken=00000000-0000-0000-0000-000000000000&nfstatusdescription=ERROR%3a+No+local+token, American Academy of Pediatrics, HealthyChildren.org, “Lawn Mower Safety” https://www.healthychildren.org/English/safety-prevention/at-home/Pages/Lawnmower-Safety.aspx American Journal of Surgery, “Epidemiology of lawn-mower related injuries in children: A 10 year review” http://www.americanjournalofsurgery.com/article/S0002-9610(16)30006-X/abstract U.S. Consumer Product Safety Commission's 2014 Fireworks Annual Report http://www.cpsc.gov//Global/Research-and-Statistics/Injury-Statistics/Fuel-Lighters-and-Fireworks/Fireworks_Report_2014.pdf Spring has finally sprung in the Utah. The weather is warmer, the days longer, the foothills are an emerald shade of green, and the trees and flowers are blooming. Everyone is getting outside as there are an unlimited number of things to do and much to explore. Because of this, it is the perfect time for a friendly reminder of how to keep your kids safe while having fun in the sun this Spring and Summer. Since I don't want to bombard you with too much information all at once, I'm going to make this a two-part series. This month's post: sun and water safety.
Spring is the time of the year that we see many sunburns as people are heading outdoors again. Because it's not super hot outside, many forget to protect themselves. The best way to protect against harmful ultraviolet radiation exposure is to cover up. For infants less than 6 months of age, avoid being in the sun and dress them in lightweight long-sleeved shirts, long pants and wide brimmed hats that shade the neck and face. If shade and clothing are not available, apply a minimal amount of sunscreen with a sun protection factor (SPF) of at least 15 (up to SPF 50) to the face and back of hands. Generally, sunscreen is not recommended for infants less than 6 months of age, but if no other options are available, a small amount is okay. For children of all ages, avoid being outside during the sun's peak intensity hours of 10:00 am and 04:00 pm. If that's unavoidable, stay in the shade and wear clothing with a tight weave, wear a light-colored hat with a wide brim and wear sunglasses that protect against both UVA and UVB rays. It is also important to apply at least an SPF 15 sunscreen on all exposed skin areas and reapply every 2 hours if swimming or sweating. Be mindful of your surroundings, water and sand (and snow for those of us in Utah!) can intensify UV rays and precipitate sunburn. Finally, be a good example and teach your children how to apply sunscreen by doing so yourself. Your children will be more eager to do what they see you doing. I'm often asked by parents which sunscreen is best because there are many brands to choose from. When choosing a sunscreen, look for one that says “broad-spectrum” on the front. This means that it designed to deter UVA and UVB rays. You also want to choose a sunscreen that is at least SPF 15. One common mistake people make when applying sunscreen is not using enough. You need to apply enough to generously cover all exposed areas of the body, including the face, ears, nose, feet, backs of the knees and hands. Another mistake many people make is not applying it soon enough before going outdoors. It is important to apply sunscreen to dry skin 30 minutes before going outside because it needs time to absorb into the skin in order to be effective. Here at ABC Pediatrics, we typically recommend Blue Lizard® sunscreen. We have found it works well on all skin types when used properly (see here: Sun Protection). Plus, an added bonus is the bottle changes colors when exposed to harmful UV rays giving you another reminder to cover-up. You're kids will surely dig that! If, despite all of your best efforts, one of your children does get a sunburn you want to make sure to keep them comfortable. Make sure he or she remains hydrated by drinking plenty of fluids. A cool bath can help soothe any inflamed skin. Be sure to keep their skin well-moisturized, but be cautious because some lotions may sting your child's already irritated skin. Aloe Vera gel or lotion can be helpful in these situations. Giving your child pain medication such as acetaminophen helps with painful sunburns. Finally, keep your child out of the sun until the sunburn has completely healed. Some reasons to seek medical attention would be any sunburn in an infant less than 1 year of age or a sunburn in an older child that is accompanied by blistering, extreme pain or fever. Now we're going to talk about getting wet. Whether it's splashing around in a pool or enjoying a boat ride on a lake, water provides endless hours of entertainment. However, if not respected properly, water fun can end in tragedy. Be sure to protect your child by following these water safety tips. First, and foremost, never ever leave a child unattended around any type of open water. This means pools, lakes, streams, rivers, ponds, spas, etc. You even need to think of things like buckets of water or coolers left out with melting ice. If the child is less than 5 years old, make sure you or another adult, are within arm's length of the child, this is called “touch-supervision”. This allows the adult in the water to be able to quickly help a child should they lose their balance and go under water. If you own a pool, make sure there is at least a 4 foot fence surrounding all four sides of the pool and that it's locked at all times with a self-closing and self-latching device that a child cannot reach. If your house exterior wall is the one of the four sides of the pool's enclosure, make sure that any doors or exits from the house (even animal doors) remain locked at all times – even better would be if they were equipped with an alarm that will sound if opened. It also wouldn't hurt considering installation of gate alarms or water surface sensors that will notify someone if somebody enters the pool area or pool itself. Make sure rescue equipment such as a shepherd's hook, a life-preserver and a portable telephone are nearby in the event of an emergency. Inflatable swimming aids, also called “floaties”, should not be used as a substitute for a life jacket as they can give parents and children a false sense of security. Formal swimming lessons can lessen the risk of drowning in children over 1 year of age, but it is important to never consider them a way of “drown-proofing” your child. Life-jackets should be worn at all times while on a boat, on docks, or near bodies of water. Make sure the life-jacket is the appropriate size for the child and verify that it's not loose and all belts are securely fastened. Finally, make sure you teach your children to never dive into water unless given the okay by an adult who has checked the depth and made sure there are no underwater objects. So, there you have it for sun and water safety. As always, don't hesitate to contact us here at ABC Pediatrics if you have further questions or concerns. Stay tuned for next month's post where I will talk about playground safety and proper helmet use. Wishing you a happy and safe spring and summer! *Information presented adapted from Health Children.org “Sun Safety” https://www.healthychildren.org/English/safety-prevention/at-play/Pages/Sun-Safety.aspx and The American Academy of Pediatrics news feature “Sun and Water Safety Tips” https://www.aap.org/en-us/about-the-aap/aap-press-room/news-features-and-safety-tips/Pages/Sun-and-Water-Safety-Tips.aspx?nfstatus=401&nftoken=00000000-0000-0000-0000-000000000000&nfstatusdescription=ERROR:+No+local+token Do you have a child that is always on the go, talks too much, won't sit still, can't seem to follow directions or complete tasks, doesn't pay attention, can't keep track of his or her things, cannot play quietly, or is forgetful? Sure, many of these qualities are just kids just being kids, especially if they are younger in age. However, if these symptoms don't improve over time and are beginning to affect your child's school, family and social life, they could be due to something called Attention deficit/Hyperactivity Disorder (ADHD).
ADHD stands for AttentionDeficit/Hyperactivity Disorder and it is a common behavioral disorder that affects approximately 10% of U.S. children ages four to seventeen. Symptoms usually arise in early childhood, and can continue throughout teenage years into adulthood. Despite numerous studies, researchers have yet to pinpoint an exact cause of ADHD. Nonetheless, these studies have suggested there is a strong genetic link because ADHD can run in families. There also is evidence to suggest that exposure to pesticides or lead in early childhood, brain injury, and prematurity and/or low birthweight may increase likelihood of having ADHD. ADHD is characterized by developmentally inappropriate levels of inattention, impulsivity and hyperactivity. It is classified into three subtypes, “primarily inattentive”, “primarily hyperactive” and “combined type” which would be inattentive and hyperactive. There is a common misconception that ADHD only applies to the child who is hyperactive, impulsive and is always bouncing off the walls. This isn't true because the calm and quiet child could also have ADHD with predominantly inattentive symptoms. In addition to subtypes, ADHD can be classified as “mild”, “moderate” or “severe”. In the same way a child may have mild asthma with symptoms occasionally affecting activities of daily living, you can also have mild ADHD. There is no single test to diagnose ADHD. It is a complex process that takes time and effort and involves collecting information from the child's parents, teachers, and health careprofessionals. The most recommended method by medical organizations is to complete an ADHD rating form by at least 2 adults from 2 different settings, usually home and school. ABC Pediatrics uses the Vanderbilt, (click here), but other institutions may use the Conners evaluation forms. In order for a diagnosis of ADHD to be made, children should have 6 or more symptoms of the disorder present for greater than 6 months and symptoms must have appeared before 12 years of age. In addition, the child's health care provider will do a thorough medical history and physical examination in order to screen for other conditions that could be affecting the child's behavior. If a diagnosis of ADHD is made, the treatment varies depending on the child's age and severity. Treatment for ADHD is multimodal, usually consisting of behavioral, educational, medical, and psychological intervention. Many parents are hesitant to put their child on medication, but it seems to be an essential part of treatment for ADHD as medications have outperformed behavioral and nutritional therapy alone in clinical trials. The medications for ADHD fall into two categories: psychostimulants and nonstimulants. Stimulants are the first line therapy as they have been the most widely studied. The effectiveness of nonstimulant medication is based on limited clinical trials and, mostly, clinical experience. The child's provider will tailor medication to the special needs of the child and his or her family with the end goal being the best possible outcome with the least amount of side effects. Most side effects are mild and short-term and include appetite suppression, insomnia, anxiety, and agitation. In the same way some parents might be hesitant to put their child on medication, they also need to be aware that there is no magic pill to cure ADHD. Medications will not control the child's behavior, but they will decrease symptoms of ADHD so the child can function more effectively at school and at home. Finally, parents need to be aware that after a diagnosis is made, it is just the beginning of a long journey ahead. The first step is to become better educated in all things ADHD. Read as much as you can and don't hesitate to contact your health care provider with any questions that may come up. Parenting a child with ADHD can be difficult, confusing and stressful. Parents may have to change the way in which they rear their children in some instances. There are a wealth of resources available and I will often direct my patient's families to the Children and Adults with Attention Deficit/Hyperactivity Disorder (CHADD) website (click here) and if you live in Utah, the Utah Academy of Child and Adolescent Psychiatry (UACAP) (click here) is great as well. Last, but not least, the following informational brochure is loaded with tips for parenting a child with ADHD (click here) As always, please do not hesitate to contact us here at ABC Pediatrics with additional questions. We are here for you! *Information provided adapted from the American Academy of Pediatrics “ADHD: Clinical Practice Guidelines for the Diagnosis, Evaluation, and Treatment of Attention Deficit/Hyperactivity Disorder in Children and Adolescents”, the Utah Academy of Child and Adolescent Psychiatry's website on ADHD, and from the Children and Adults with Attention Deficit/Hyperactivity Disorder's website. If you've been reading news headlines the past month you probably know two things for sure. First, we are in an election year and we will keep hearing why such and such candidate is better than so and so candidate until the talking heads are blue in the face. And, two, that a mysterious virus by the name of Zika is wreaking havoc in much of the Southern hemisphere. While I can't help you with your decision on who to vote for in November of 2016, I can help shed some light on Zika and how it affects you and your family.
Zika is a virus that can cause symptoms of fever, rash, pink eye and joint pain. These symptoms usually last about one week and are typically mild. Rarely are the symptoms so severe that they require hospitalization. It can be spread from person to person via the bite of a mosquito and through sexual contact, from an infected male to his partner. The Centers for Disease Control and Prevention (CDC) is still investigating if it can be spread via saliva and urine, but that has yet to be determined. So, why all the fuss then? The World Health Organization (WHO) has issued a public health emergency as it investigates the possible link of babies born with abnormally small heads, known as microcephaly, and other birth defects, and the Zika virus. Additionally, there may be a possible link between Gullian Barre syndrome, a disorder characterized by progressive muscle weakness that can lead to entire body paralysis, and the Zika virus. As of now, it is unknown whether the increase in microcephaly cases or the cases of Gullian Barre are directly caused by Zika. It is because of the possible link of Zika to microcephaly that the CDC has issued warnings to pregnant women and women who are trying to get pregnant. If you or your partner is pregnant or trying to get pregnant, it would be best to hold off on travel to areas with Zika (http://wwwnc.cdc.gov/travel/page/zika-information). If you must travel to these places, first talk to your doctor before you go and be sure to take special precautions while there -- specifically, avoid getting mosquito bites. Also, if you do travel to one of these areas while pregnant, it is recommended you get tested between 2 and 12 weeks after your return, even if you are not showing symptoms. I’ve received some questions in the last few weeks from families who are traveling to areas with Zika and what they need to do to protect themselves. The best way to prevent you or your family from getting Zika virus is to prevent against mosquito bites. Make sure you wear clothing with long sleeves and long pants that have embedded Permethrin, use insect repellants, and sleep in places with screens or air-conditioning, or use mosquito netting over your bed. Thankfully, as of right now, there have been no confirmed Zika cases acquired in the United States (U.S). All the cases confirmed in the U.S. have been acquired in other countries with Zika. There is some worry that with warmer weather on the horizon the mosquitos that carry Zika will make their way North, although for right now it’s not the case. Currently there is no vaccine or treatment for Zika, so the best way to avoid the effects of Zika is not getting in the first place. Researchers are working on developing a vaccine, although that could take years before it is available to the masses. Check out the CDC's website for more detailed and up-to-date information. Or, if you have more specific questions, don’t hesitate to contact us at ABC Pediatrics. We are happy to help! *Information presented adapted from Center for Disease Control and Prevention information on Zika http://www.cdc.gov/zika/index.html I talk about poop all the time at work. Honestly, I don't think a day goes by at our office where I don't talk about it. I've received many weird looks from my patients (and their parents) when I ask what their poop looks like, but all joking aside, the frequency, the amount, and the consistency of your child's bowel movements can tell us a lot about his or her health.
Bowel patterns differ from child to child, but on average your child should be having a painless, soft, bowel movement every day to every other day. Bowel movements should never be hard or painful. If that's the case, your child could be constipated. Now, depending on your child's age, the days in between bowel movements may vary. For example, an exclusively breast-fed infant older than 1 month of age may go up to one week without a bowel movement – breast milk is absorbed really well so there isn't much left to come out. As a medical professional I wouldn't be concerned if an infant goes seven days in between bowel movements as long as he or she is otherwise doing well and as long as it's soft. So, what are some other signs that your child could be suffering from constipation? Here are a few examples:
The best way to treat constipation is to prevent it from happening in the first place. A healthy diet, staying hydrated and daily, physical activity will all help make this possible. Make sure your child's diet is rich in fruits and vegetables. Avoid consuming heavy, fatty foods often – like pizza and mac 'n' cheese to name a couple. If it's too late for prevention and it seems your child is constipated, then really pushing foods that are high in fiber may help. For example, encouraging your child to eat those fruits that begin with P: peaches, pears, and plums are very effective in helping your child have a bowel movement. Apples, with the skin on, are also great. There's actually truth behind the “apple a day” adage after all. Not only is what your child eats important, but the timing of when he or she eats it is important as well. For example, if your child wants to have a slice of pizza or a bowl of mac 'n' cheese, pairing it with a big green salad and an apple as dessert will help prevent them from getting constipated. You can think of the apple and salad as helping push the other “heavier” food along. Make sure your child is hydrated and drinking enough water each day. All of that good fiber needs water, if not, constipation can worsen. Finally, at least 30 minutes of daily, physical activity, can help constipation. Whether that's a game of basketball or a leisurely hike on our local trails, getting your child moving will help get those bowels moving likewise. Well, that's my "scoop" on poop. In conclusion, many children suffer from mild constipation, but that can usually be fixed with diet modification. If a change in diet and exercise aren't helping, and you have any other concerns or questions specific to your child, contact us here at ABC Pediatrics. We are here to help and we would be happy to see you! If you'd like to watch a short video about what we'll likely discuss at your child's appointment, click here. *Information presented adapted from Healthy Children.org “Constipation” www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Constipation |
Mary-Faith Fuller, CPNPI am a Pediatric Nurse Practitioner who has worked at ABC Pediatrics since January 2014. Archives
June 2020
Categories |
Copyright © 2005-2023 │ 6360 S 3000 E Ste 230 Cottonwood Heights UT 84121 │ 801-523-3030
|
Where we treat you like family!
|








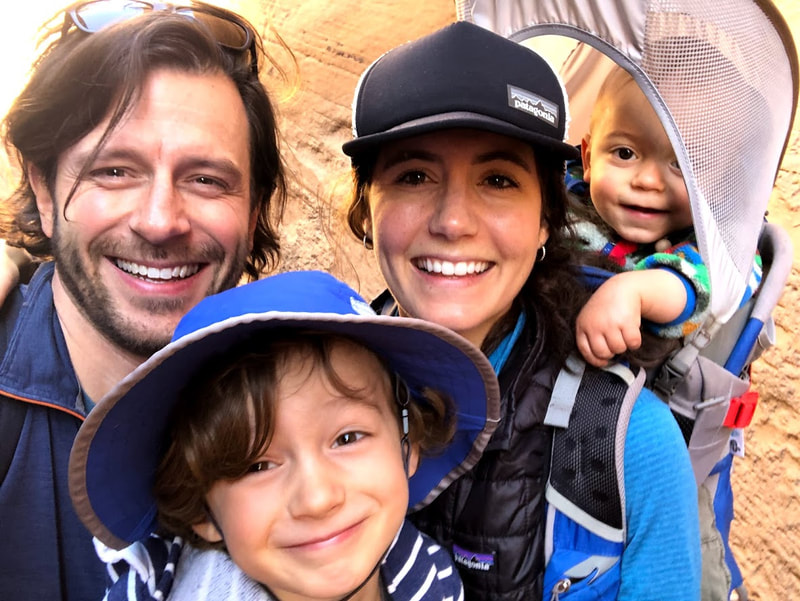
 RSS Feed
RSS Feed




